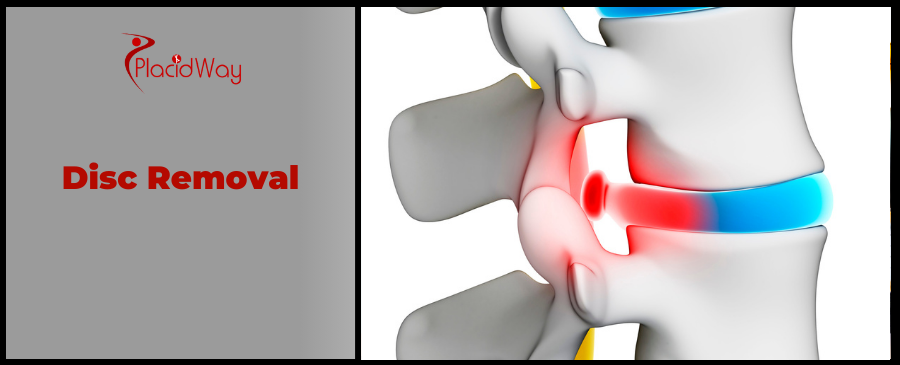
Finding Relief Abroad: Your Guide to Disc Removal Surgery
Living with persistent back pain, radiating leg pain (sciatica), numbness, or weakness can be debilitating, significantly impacting your quality of life. When these symptoms stem from a herniated or bulging disc pressing on your spinal nerves, and conservative treatments like medication, physical therapy, or injections no longer offer relief, disc removal surgery—known medically as a discectomy—might be the path to reclaiming your comfort and mobility.
This procedure involves carefully removing the damaged portion of a spinal disc to alleviate pressure on the affected nerve. For many, it's a life-changing intervention that allows them to return to daily activities without chronic discomfort. However, the decision to undergo surgery, especially in a different country, comes with many questions about cost, safety, quality, and recovery.
This comprehensive guide is designed to empower you with the knowledge needed to make informed decisions about disc removal surgery, whether you're considering treatment locally or exploring the significant benefits of medical tourism. We’ll delve into everything from understanding your condition and the types of procedures available, to comparing costs globally and navigating the process of seeking care abroad, ensuring you find the best solution for your unique needs.
What are the Symptoms of a Herniated Disc?
A herniated disc occurs when the soft, jelly-like center of a spinal disc pushes through a tear in its tougher outer casing. This can irritate nearby nerves, leading to a range of uncomfortable and sometimes debilitating symptoms. Recognizing these signs is the first step toward seeking appropriate treatment.
- Localized Back or Neck Pain: Often, the initial symptom is a sharp or burning pain in the area of the herniated disc, which can worsen with movement, coughing, or sneezing.
- Radiating Pain (Sciatica): If the herniated disc is in the lower back, pain may radiate down the buttock, leg, and even into the foot. This is commonly known as sciatica. If in the neck, pain can spread to the shoulder, arm, and hand.
- Numbness or Tingling: Patients often describe sensations of "pins and needles" or numbness in the area served by the affected nerve.
- Muscle Weakness: The compromised nerve signal can lead to weakness in the muscles it supplies, making it difficult to lift objects, walk, or perform fine motor tasks.
- Loss of Reflexes: In some severe cases, reflexes in the affected limb may be diminished or absent.
- Bowel or Bladder Dysfunction: This is a rare but serious symptom (Cauda Equina Syndrome) and requires immediate medical attention.
These symptoms can vary in intensity from mild discomfort to severe, incapacitating pain. If you experience any of these, especially if they persist or worsen, consulting a medical professional is crucial for an accurate diagnosis.
What Causes a Herniated Disc and What are the Risk Factors?
Understanding the root causes and risk factors behind a herniated disc can help in prevention and effective management. While sometimes it can occur spontaneously, often it's a result of various stressors on the spine.
- Age: Discs naturally degenerate and lose water content as we age, making them less flexible and more prone to tearing. This is why herniated discs are most common in people between 30 and 50 years old.
- Trauma or Injury: A sudden impact, fall, or twisting injury can cause a disc to herniate.
- Improper Lifting Techniques: Using your back muscles instead of your legs to lift heavy objects can place excessive strain on your spinal discs.
- Obesity: Excess body weight puts increased stress on the discs in your lower back, making them more susceptible to herniation.
- Repetitive Motions: Certain occupations or activities that involve repeated bending, twisting, or lifting can contribute to disc wear and tear.
- Genetics: There may be a genetic predisposition to disc degeneration, meaning some individuals are simply more prone to herniation.
- Smoking: Nicotine can reduce oxygen supply to the spinal discs, accelerating their degeneration and making them more fragile.
- Sedentary Lifestyle: Lack of regular exercise can lead to weak core muscles, which provide less support for the spine.
While some factors like age and genetics are beyond our control, adopting healthy habits such as maintaining a healthy weight, exercising regularly, and practicing proper lifting techniques can significantly reduce your risk.
What Types of Disc Removal Surgery are There?
Disc removal surgery, or discectomy, has evolved significantly, offering several approaches to address a herniated disc. The choice of procedure depends on factors like the disc's location, the severity of the herniation, and the surgeon's expertise.
- Microdiscectomy:
- Description: This is the most common type of disc removal surgery. It's a minimally invasive procedure performed using a special microscope to view the spinal nerves and disc. A small incision (1-2 inches) is made, and muscles are moved aside rather than cut.
- Benefit: Less muscle damage, smaller scar, quicker recovery, and often an outpatient procedure.
- When Used: Primarily for lumbar (lower back) herniated discs causing sciatica.
- Endoscopic Discectomy:
- Description: Even more minimally invasive than microdiscectomy, this procedure uses a tiny camera (endoscope) inserted through a very small incision (less than an inch). The surgeon views the spine on a monitor and uses specialized instruments to remove the disc fragment.
- Benefit: Minimal tissue disruption, faster recovery, often outpatient, reduced pain.
- When Used: For specific types of herniations, often in the lumbar spine.
- Open Discectomy:
- Description: This traditional approach involves a larger incision to directly access the spine. It's less common now due to advancements in minimally invasive techniques.
- Benefit: Allows the surgeon a wider field of view for complex cases.
- When Used: Reserved for more complex or multi-level herniations, or when minimally invasive options are not suitable.
- Artificial Disc Replacement (ADR):
- Description: While not strictly "disc removal," ADR involves removing the entire damaged disc and replacing it with an artificial disc device. This aims to maintain spinal mobility, unlike fusion surgery.
- Benefit: Preserves motion in the spinal segment, potentially preventing adjacent segment degeneration.
- When Used: For specific cases of degenerative disc disease in the neck or lower back where motion preservation is desired.
Your surgeon will discuss the most appropriate procedure based on your specific condition and medical history. Modern techniques prioritize minimal invasiveness to reduce recovery time and post-operative discomfort.
Am I a Candidate for Disc Removal Surgery?
Deciding if disc removal surgery is right for you is a crucial step that involves a thorough evaluation by a spine specialist. While it offers significant relief for many, it's generally not the first line of treatment.
You may be considered a candidate for disc removal surgery if:
- Conservative Treatments Have Failed: You've diligently tried non-surgical methods like physical therapy, medication, steroid injections, and chiropractic care for at least 6-12 weeks, and your symptoms persist or worsen.
- Persistent, Severe Pain: Your pain is severe enough to significantly interfere with your daily activities, work, and quality of life, and it hasn't improved with non-surgical options.
- Neurological Deficits: You are experiencing progressive muscle weakness, numbness, or loss of sensation in your limbs, indicating nerve compression.
- Imaging Confirms Disc Herniation: MRI or CT scans clearly show a herniated disc that correlates with your symptoms and is pressing on a spinal nerve.
- Cauda Equina Syndrome: This is a medical emergency characterized by progressive weakness in both legs, numbness in the saddle area (groin, buttocks), and bowel or bladder dysfunction. Immediate surgery is required.
- Good General Health: You are in reasonably good health to undergo surgery and anesthesia, with no uncontrolled medical conditions that would significantly increase surgical risks.
- Realistic Expectations: You understand the potential benefits and risks of the surgery, and have realistic expectations about recovery and outcomes.
Your surgeon will assess your symptoms, conduct a physical examination, and review imaging studies to determine if you are a suitable candidate and which surgical approach would be most effective for your specific condition.
What is the Recovery Time for Disc Removal Surgery?
The recovery time after disc removal surgery largely depends on the type of procedure, your overall health, and how well you adhere to post-operative instructions. However, many patients experience a relatively quick return to activity, especially with minimally invasive techniques.
- Immediately After Surgery (Hospital Stay):
- Most microdiscectomy patients go home the same day or within 24 hours.
- Pain management will be provided, and you'll be encouraged to walk short distances soon after surgery.
- First 1-2 Weeks:
- Focus on rest and light activity. Avoid bending, twisting, or lifting.
- Pain at the incision site is normal. Nerve pain may still be present but should gradually improve.
- You'll likely start gentle walking and may begin light physical therapy exercises.
- 2-6 Weeks:
- Physical therapy becomes more intensive, focusing on core strengthening, flexibility, and proper posture.
- Most patients can return to light office work within 2-4 weeks.
- Avoid heavy lifting (typically more than 10-15 pounds).
- 6 Weeks - 3 Months:
- Gradual return to more strenuous activities, with continued physical therapy.
- Athletes or those with physically demanding jobs may require longer, up to 3-6 months, for a full return.
- Your surgeon will clear you for specific activities based on your progress.
Full recovery, where you feel completely back to normal, can take anywhere from a few months to a year. Adhering to your physical therapy program is paramount for long-term success and to prevent recurrence. Listen to your body and follow your surgeon's guidance meticulously.
What are the Risks and Side Effects of Disc Removal Surgery?
While disc removal surgery is generally safe and effective, like any surgical procedure, it carries potential risks and side effects. It's important to discuss these thoroughly with your surgeon to make an informed decision.
- Infection: Though rare, any surgery carries a risk of infection at the incision site or within the spine.
- Bleeding: Some bleeding is normal, but excessive bleeding requiring a transfusion is a potential, though uncommon, risk.
- Nerve Damage: While the goal is to relieve nerve compression, there's a small risk of incidental nerve damage during the procedure, which could lead to new or worsened numbness, weakness, or pain.
- Dural Tear (CSF Leak): The dura is the tough membrane covering the spinal cord. A tear can occur during surgery, leading to a cerebrospinal fluid (CSF) leak. This is usually repaired during surgery and typically resolves without long-term issues.
- Recurrent Herniation: There's a small chance (about 5-10%) that the same disc could herniate again at the same level in the future, potentially requiring another surgery.
- Failed Back Surgery Syndrome (FBSS): This term refers to persistent or new back pain after surgery, which can be due to various factors not directly related to the initial surgery's success, such as scar tissue formation or progression of degenerative changes.
- Anesthesia Risks: Risks associated with general anesthesia include adverse reactions, respiratory problems, or cardiovascular events.
- Blood Clots: Deep vein thrombosis (DVT) in the legs, which can potentially travel to the lungs (pulmonary embolism), is a rare but serious risk.
Your surgeon will take precautions to minimize these risks, and your medical team will monitor you closely during and after the procedure. Open communication with your doctor about any concerns is vital.
How Much Does Disc Removal Surgery Cost Globally? (Cost Comparison)
The cost of disc removal surgery can vary dramatically depending on the country, the clinic's reputation, the surgeon's experience, the type of procedure, and whether it's performed as an inpatient or outpatient procedure. Medical tourism has become a popular option for those seeking high-quality care at a more affordable price.
Here's an estimated cost comparison for a microdiscectomy, one of the most common disc removal procedures:
| Country | Estimated Cost (USD) | Notes |
|---|---|---|
| United States | $25,000 - $60,000+ | Highly variable, depends on insurance, facility, and surgeon. |
| United Kingdom | $15,000 - $35,000+ | Private sector costs. NHS waiting lists can be long. |
| Canada | $15,000 - $30,000+ | Similar to UK private costs, but public system has long wait times. |
| Mexico | $6,000 - $12,000 | Popular for proximity to US, significant savings. |
| Turkey | $7,000 - $15,000 | Renowned for modern facilities and experienced surgeons. |
| India | $5,000 - $10,000 | Very competitive pricing, high-quality hospitals. |
| Thailand | $8,000 - $16,000 | Excellent medical infrastructure, popular for medical tourism. |
Please note: These are estimated ranges and actual costs can vary. They typically include surgeon's fees, anesthesia, hospital stay, and basic post-operative care, but may not include flights, accommodation, or extensive rehabilitation. Always request an all-inclusive quote.
Why Consider Disc Removal Surgery Abroad?
The decision to seek medical treatment in another country, often referred to as medical tourism, is growing in popularity, and for good reason. For disc removal surgery, the advantages can be substantial.
- Significant Cost Savings: As seen in the table above, the most compelling reason is often the dramatic reduction in cost. Patients can save anywhere from 50% to 80% on total procedure costs compared to Western countries, even after factoring in travel and accommodation.
- Access to Immediate Care / Shorter Wait Times: In countries with universal healthcare systems, long waiting lists for specialist consultations and surgeries can delay much-needed relief. Abroad, patients can often schedule their procedure much faster.
- Access to Specialized Expertise and Advanced Technology: Many international hospitals specialize in spinal surgery and boast world-class surgeons trained in the latest minimally invasive techniques. They are often equipped with state-of-the-art diagnostic and surgical technology that may not be readily available or affordable in one's home country.
- Higher Quality of Care and Personalized Attention: Medical tourism often means receiving care in private hospitals known for excellent patient-to-staff ratios, luxurious recovery suites, and comprehensive, personalized attention, sometimes exceeding standards found at home.
- Combine Treatment with a Vacation: For some, the opportunity to recover in a beautiful, serene environment, effectively combining necessary surgery with a period of rest and cultural exploration, is an added appeal.
Choosing to go abroad requires careful planning, but the benefits—especially for a procedure like disc removal—can be life-changing, offering relief from pain without financial strain.
Which Countries Offer Best Value for Disc Removal Surgery?
When seeking disc removal surgery abroad, certain countries have emerged as leading destinations, offering a compelling combination of affordability, quality care, and an established infrastructure for medical tourism.
- Mexico:
- Why: Close proximity to the U.S. and Canada, making travel convenient. Offers advanced private hospitals and highly skilled, U.S.-trained surgeons.
- Value: Excellent cost-to-quality ratio, with savings often around 50-70%.
- Turkey:
- Why: A bridge between Europe and Asia, Turkey boasts numerous JCI-accredited hospitals (Joint Commission International) and experienced neurosurgeons. It's particularly popular for patients from Europe and the Middle East.
- Value: Very competitive pricing, state-of-the-art facilities, and often comprehensive packages.
- India:
- Why: A global leader in medical tourism, offering world-class healthcare at a fraction of Western costs. Indian hospitals are known for cutting-edge technology and highly qualified, English-speaking doctors.
- Value: Among the lowest costs for high-quality spinal surgeries, with savings up to 80% or more.
- Thailand:
- Why: Renowned for its hospitality, Thailand also has a well-developed medical tourism industry with JCI-accredited hospitals and excellent patient care. It combines recovery with a pleasant travel experience.
- Value: High-quality medical care at significantly lower prices than Western countries, often with a focus on patient comfort and comprehensive services.
- South Korea:
- Why: Known for its technological advancements and highly specialized medical centers, particularly in spine care. Korean hospitals are at the forefront of medical innovation.
- Value: While slightly higher in cost than some other Asian destinations, it offers unparalleled technological sophistication and highly specialized care.
These countries not only provide affordable solutions but also maintain rigorous standards, often with international accreditations, ensuring patient safety and successful outcomes.
What to Expect When Traveling for Disc Removal Procedure Abroad?
Embarking on a medical journey abroad might seem daunting, but with proper planning, it can be a smooth and rewarding experience. Here's a general overview of what to expect:
- Initial Consultation & Research:
- Start by researching destinations and clinics. Use a medical tourism facilitator like PlacidWay to help you gather information, compare options, and get personalized quotes.
- You'll likely have virtual consultations (video calls) with potential surgeons to discuss your case, review medical records, and get a preliminary diagnosis and treatment plan.
- Travel Arrangements:
- Once you've chosen a clinic and surgeon, coordinate travel dates. Book flights, and decide on accommodation (many medical tourism packages include this, or clinics have arrangements).
- Ensure your passport is valid and check visa requirements for your chosen country.
- Pre-Operative Care:
- Upon arrival, you'll undergo in-person consultations, further diagnostic tests (MRI, X-rays), and a comprehensive medical evaluation to ensure you're fit for surgery.
- You'll meet the surgical team and anesthesiologist.
- The Procedure:
- On the day of surgery, you'll be admitted to the hospital. The disc removal procedure will be performed as planned.
- The hospital staff will be experienced in caring for international patients and often provide translators.
- Post-Operative Recovery & Rehabilitation:
- After surgery, you'll spend time recovering in the hospital, often with excellent nursing care.
- Initial physical therapy and mobility exercises will begin.
- Before returning home, you'll have follow-up appointments with your surgeon, receive detailed post-op instructions, medication, and a plan for continued rehabilitation.
- Return Home:
- Travel will need to be carefully planned around your recovery. Avoid heavy lifting and long periods of sitting during the journey.
- Continue your prescribed physical therapy and follow-up with your local doctor as advised.
Medical tourism facilitators play a crucial role in streamlining this process, handling many logistical details so you can focus on your health.
How to Ensure Safety and Quality for Disc Removal Abroad?
The primary concern for any patient considering surgery, especially abroad, is safety and quality of care. It's essential to perform thorough due diligence. Here's how to ensure you're making a safe and informed choice:
- Choose JCI-Accredited Hospitals: Look for hospitals that have been accredited by the Joint Commission International (JCI). This is a globally recognized gold standard for patient safety and quality of care.
- Verify Surgeon Credentials and Experience:
- Ensure your surgeon is board-certified in neurosurgery or orthopedic spine surgery.
- Inquire about their experience with disc removal procedures, specifically the type you need.
- Check their professional affiliations and if they have undergone international training.
- Review Patient Testimonials and Reviews: Seek out real patient experiences and reviews. Look for consistent positive feedback regarding outcomes, care, and overall experience.
- Utilize Reputable Medical Tourism Facilitators (like PlacidWay):
- These services vet clinics and surgeons, simplify logistics, provide transparent pricing, and offer support throughout your journey.
- They can help you communicate with doctors, translate documents, and arrange travel details.
- Transparent Communication: Ensure the clinic provides clear, detailed information about the procedure, risks, recovery, and an all-inclusive cost breakdown with no hidden fees.
- Post-Operative Care Plan: Confirm that a clear post-operative care plan is provided, including recommendations for follow-up with your local doctor and details on how to contact the surgical team if issues arise after your return.
- Travel Insurance: Consider comprehensive travel insurance that includes medical evacuation and coverage for complications, if available.
By taking these steps, you can significantly mitigate risks and increase your confidence in receiving high-quality, safe medical care abroad.
What are Patient Success Stories from Disc Removal Abroad?
The true measure of a medical journey often lies in the experiences and outcomes of those who have walked the path before you. Patient success stories highlight not just the medical efficacy but also the profound impact on quality of life.
Example 1: The Active Retiree from Canada
"Margaret, a 62-year-old from Toronto, faced excruciating sciatica due to a lumbar herniation. After a year of physiotherapy and injections with no significant improvement, and facing a 12-month wait for surgery at home, she explored options in Turkey. She underwent a microdiscectomy in Istanbul. 'The clinic was pristine, the surgeon incredibly skilled, and the recovery seamless,' she shared. 'Within weeks, I was walking pain-free, and now I'm back to gardening and playing with my grandchildren. The cost was less than half of what a private clinic in Canada would have charged, and I got my life back so much sooner.'"
Example 2: The Young Professional from the UK
"James, 35, from London, developed severe lower back pain and leg weakness that threatened his career as a graphic designer. Frustrated by prolonged waiting lists and high private costs in the UK, he chose a JCI-accredited hospital in India for an endoscopic discectomy. 'From the moment I landed, everything was taken care of,' James recounted. 'The surgical precision and aftercare were exceptional. Not only did I save a fortune, but I also felt like a VIP. My pain is gone, and I'm back at my desk, more productive than ever, without the constant distraction of discomfort.'"
These stories are common threads in the narrative of medical tourism for disc removal. Patients often report:
- Significant Pain Relief: The most immediate and desired outcome, allowing a return to a normal, active life.
- Improved Mobility and Function: Regaining the ability to walk, bend, lift, and participate in hobbies without limitations.
- Enhanced Quality of Life: Freedom from chronic pain improves mood, sleep, and overall well-being.
- Peace of Mind: The relief of having a debilitating condition effectively treated, often much faster and more affordably than at home.
Such testimonials underscore the potential for successful outcomes and a renewed lease on life for those who choose international care for their disc removal surgery.
Take the Next Step with PlacidWay
Ready to explore treatment options abroad? Discover top clinics, compare prices, and get a free quote tailored to your needs with PlacidWay.
Orthopedic Surgery Abroad, Knee Sugery Abroad




.png)
.png)
.png)
.png)

Share this listing