
Find Lasting Relief: Your Guide to Hemorrhoids Removal Options
Dealing with hemorrhoids can be a deeply uncomfortable, sometimes painful, and often embarrassing experience that impacts your daily life and overall well-being. If you've tried lifestyle changes and over-the-counter remedies without success, you're likely searching for a more permanent solution. You're not alone in wondering, "How do I finally get rid of these hemorrhoids?" or "What are the best hemorrhoid treatment options available?"
Hemorrhoids are essentially swollen veins in the anus and lower rectum, similar to varicose veins. They can be internal (inside the rectum) or external (under the skin around the anus). While many cases resolve with simple care, persistent or severe hemorrhoids can lead to chronic pain, itching, bleeding, and even prolapse – where internal hemorrhoids protrude outside the anus. When symptoms become debilitating and conservative treatments fail, hemorrhoid removal becomes a necessary step toward regaining comfort and quality of life.
This comprehensive guide will explore everything you need to know about hemorrhoid removal, from understanding your symptoms and causes to the various treatment options. We’ll delve into recovery expectations, potential risks, and a crucial aspect for many patients: the global cost comparison. For those considering medical travel, we’ll also answer common questions about seeking hemorrhoid treatment abroad, including how to find the best value, ensure safety, and what to expect during your journey. Our goal is to empower you with the knowledge to make an informed decision and find the lasting relief you deserve.
What are the common symptoms of hemorrhoids that might require removal?
Recognizing the symptoms of hemorrhoids is the first step towards seeking effective treatment. While mild hemorrhoids might cause minimal discomfort, those requiring removal often present with more significant and persistent issues. Here are the key signs to watch for:
- Bleeding: This is one of the most common symptoms. You might notice bright red blood on toilet paper after a bowel movement, in the toilet bowl, or on your stool. It’s usually painless bleeding.
- Pain or Discomfort: Especially with external hemorrhoids or thrombosed hemorrhoids (where a blood clot forms), you can experience significant pain, aching, or soreness around the anus.
- Anal Itching or Irritation: Hemorrhoids can cause intense itching (pruritus ani) around the anal area, leading to further irritation from scratching.
- Swelling or a Lump: External hemorrhoids often feel like a sensitive, tender lump or swelling around the anus. Prolapsed internal hemorrhoids can also present as a soft, moist pad of tissue protruding from the anus.
- Mucus Discharge: Internal hemorrhoids can sometimes lead to the discharge of mucus, which can further irritate the skin.
- Bowel Movement Issues: A feeling of fullness in the rectum even after a bowel movement, or difficulty cleaning the anal area due to swelling.
If you experience any of these symptoms, especially persistent bleeding or severe pain, it’s crucial to consult a doctor. While these symptoms often point to hemorrhoids, they can also indicate more serious conditions.
What causes hemorrhoids and what are the main risk factors?
Hemorrhoids develop when the veins around your anus and rectum become stretched and swollen under pressure. Understanding the causes and risk factors can help in prevention and effective management:
- Straining During Bowel Movements: This is a major culprit. Excessive straining, often due to constipation, puts immense pressure on the veins.
- Chronic Constipation or Diarrhea: Both extremes can irritate the anal canal and lead to straining or frequent bowel movements, contributing to hemorrhoid formation.
- Prolonged Sitting: Spending long periods sitting on the toilet or even just sitting for extended durations can increase pressure on the anal veins.
- Pregnancy: The growing uterus puts pressure on the pelvic veins. Hormonal changes during pregnancy also relax the veins, making them more susceptible to swelling.
- Obesity: Carrying excess weight can increase pressure in the abdomen, which in turn puts pressure on the rectal veins.
- Low-Fiber Diet: A diet lacking fiber leads to harder stools and contributes to constipation, necessitating more straining.
- Heavy Lifting: Repeatedly lifting heavy objects can increase abdominal pressure.
- Aging: As you age, the tissues supporting the veins in your rectum and anus can weaken and stretch.
By addressing these underlying causes and modifying lifestyle factors, you can often prevent or alleviate hemorrhoid symptoms. However, for established and severe cases, intervention is often needed.
What types of hemorrhoid removal procedures are available?
When conservative treatments aren't enough, various procedures can effectively remove or reduce hemorrhoids. These range from minimally invasive office procedures to more significant surgical interventions:
Minimally Invasive Office Procedures (for internal hemorrhoids, Grades I-III):
- Rubber Band Ligation: A small rubber band is placed around the base of an internal hemorrhoid, cutting off its blood supply. The hemorrhoid withers and falls off within about a week, usually during a bowel movement. This is one of the most common and effective treatments.
- Sclerotherapy: A chemical solution is injected into the hemorrhoid, causing it to shrink and scar.
- Infrared Coagulation (IRC): A device uses infrared light to create scar tissue, which cuts off the blood supply to the hemorrhoid, causing it to shrink.
Surgical Procedures (for larger, prolapsed, or severe hemorrhoids, Grades III-IV):
- Hemorrhoidectomy: This is the traditional surgical removal of external hemorrhoids and prolapsing internal hemorrhoids. It's highly effective but involves a longer and often more painful recovery. It's often considered the most definitive treatment for severe cases.
- Stapled Hemorrhoidopexy (PPH): Also known as procedure for prolapse and hemorrhoids, this procedure uses a stapling device to remove a ring of tissue above the hemorrhoids, lifting and repositioning them, and reducing their blood supply. It's often less painful than a traditional hemorrhoidectomy and has a quicker recovery, though it may have a higher recurrence rate for some.
- Transanal Hemorrhoidal Dearterialization (THD) / Hemorrhoidal Artery Ligation (HAL): This procedure uses a Doppler ultrasound to identify the arteries supplying blood to the hemorrhoids. The arteries are then ligated (tied off), cutting off the blood flow. This causes the hemorrhoids to shrink. Often, a "mucopexy" (lifting and stitching the prolapsed tissue) is performed concurrently. THD is considered less invasive than traditional surgery with less post-operative pain.
The choice of procedure depends on the type, size, and severity of the hemorrhoids, as well as the patient's overall health and preferences.
Who is eligible for hemorrhoid removal and when is it recommended?
Not everyone with hemorrhoids needs a removal procedure. Many cases can be managed effectively with diet changes, increased fiber intake, stool softeners, and topical creams. However, surgical or procedural intervention becomes necessary when:
- Conservative Treatments Fail: If symptoms like pain, bleeding, and itching persist despite dietary adjustments, lifestyle changes, and over-the-counter or prescription medications.
- Prolapsed Hemorrhoids: Internal hemorrhoids that prolapse (protrude from the anus) and cannot be easily pushed back in (Grade III) or remain permanently prolapsed (Grade IV) almost always require intervention.
- Persistent Bleeding: Chronic blood loss can lead to anemia and significantly impact quality of life.
- Severe Pain: Especially with external thrombosed hemorrhoids, which can cause excruciating pain.
- Large Internal Hemorrhoids: Even if not prolapsed, very large internal hemorrhoids can cause significant discomfort and bleeding.
- Impaired Quality of Life: When hemorrhoids interfere with daily activities, hygiene, or cause significant distress.
A specialist, such as a gastroenterologist or a colorectal surgeon, will assess your specific condition, including the grade of your hemorrhoids, to determine the most appropriate course of action.
What is the typical recovery time and what can I expect after hemorrhoid surgery?
Recovery is a crucial part of the healing process, and what you can expect largely depends on the type of procedure performed:
- Minimally Invasive Procedures (Ligation, Sclerotherapy, IRC):
- Recovery Time: Often a few days to a week. Most people can return to normal activities immediately or within 1-2 days.
- Expectations: You might feel some mild discomfort, fullness, or a dull ache. There might be some light bleeding, especially when the hemorrhoid falls off (after banding). Pain is usually minimal and manageable with over-the-counter pain relievers.
- Surgical Procedures (Hemorrhoidectomy, PPH, THD):
- Recovery Time:
- Traditional Hemorrhoidectomy: This is generally the longest and most painful recovery, typically 2-4 weeks, sometimes longer for full comfort.
- Stapled Hemorrhoidopexy (PPH) & THD: Generally less painful and a quicker recovery than traditional surgery, often 1-2 weeks before returning to light activities, with full recovery within 3-4 weeks.
- Expectations:
- Pain: Expect significant pain, especially after a traditional hemorrhoidectomy. This will be managed with prescription pain medication. It will gradually subside.
- Bleeding & Discharge: Some bleeding, spotting, and clear or yellowish discharge are normal, especially after bowel movements.
- Swelling: The area might be swollen initially.
- Bowel Movements: The first bowel movement can be particularly daunting and painful. Stool softeners and a high-fiber diet are crucial.
- Hygiene: Sitz baths (soaking in warm water) are highly recommended for pain relief and cleanliness.
- Activity: Avoid heavy lifting and strenuous activity for several weeks. Gradually increase activity as tolerated.
- Recovery Time:
Following your surgeon's post-operative instructions diligently is key to a smooth recovery and successful outcome.
What are the potential risks and side effects of hemorrhoid removal procedures?
As with any medical procedure, hemorrhoid removal carries some potential risks and side effects, though serious complications are rare:
- Pain: Post-operative pain is the most common side effect, varying in intensity depending on the procedure.
- Bleeding: Some bleeding is normal, but excessive or prolonged bleeding may require medical attention.
- Infection: Though rare, infection at the surgical site can occur.
- Urinary Retention: Difficulty urinating after surgery due to pain or anesthesia is possible, usually temporary.
- Fecal Impaction: Hard stools can become stuck in the rectum, often due to pain avoidance or inadequate fiber/fluid intake post-op.
- Anal Stricture (Narrowing): Scarring after extensive tissue removal can sometimes lead to a narrowing of the anal canal, making bowel movements difficult. This is more common with traditional hemorrhoidectomy.
- Fecal Incontinence: Very rarely, nerve or muscle damage can lead to difficulty controlling gas or stool, though this is extremely uncommon with modern techniques.
- Recurrence: Hemorrhoids can potentially return, especially if underlying causes (like chronic straining) are not addressed.
Your surgeon will discuss these risks with you and take precautions to minimize them. Choosing an experienced surgeon and following post-operative care instructions are vital for reducing the likelihood of complications.
How much does hemorrhoid removal cost worldwide?
The cost of hemorrhoid removal can be a major factor for many patients. Prices fluctuate widely based on the type of procedure, the complexity of the case, the clinic's location, the surgeon's fees, and whether it's performed in an outpatient setting or hospital. Medical tourism offers a compelling option for significant cost savings without compromising on quality.
Estimated Cost Comparison Table for Hemorrhoid Removal (Surgical Procedures)
| Procedure Type | Country | Estimated Cost Range (USD) |
|---|---|---|
| Rubber Band Ligation / Sclerotherapy (per session) | USA | $500 - $1,500 |
| UK | $400 - $1,000 | |
| Mexico / India / Turkey | $150 - $500 | |
| Thailand | $200 - $600 | |
| Hemorrhoidectomy / PPH / THD | USA | $4,000 - $10,000+ |
| UK | $3,000 - $7,000 | |
| Mexico | $1,800 - $4,500 | |
| India / Turkey | $1,500 - $4,000 | |
| Thailand | $2,000 - $5,000 |
*Prices are estimates and can vary based on clinic, surgeon, specific procedure variant, and included services (anesthesia, facility fees, pre/post-op care). It's crucial to get a personalized quote.
Why should I consider hemorrhoid removal abroad for better value and care?
The concept of medical tourism for procedures like hemorrhoid removal is gaining popularity for several compelling reasons:
- Significant Cost Savings: As seen in the table above, the primary driver for many is the substantial reduction in cost, often 50-70% less than in Western countries like the USA, UK, or Canada, without sacrificing quality.
- Access to Advanced Techniques: Some international clinics specialize in particular advanced or less invasive hemorrhoid treatments (like THD or specific laser techniques) that may not be widely available or as affordable in one's home country.
- Reduced Waiting Times: In countries with universal healthcare systems, waiting lists for non-emergency procedures can be long. Traveling abroad often allows for immediate scheduling.
- Privacy and Discretion: For some, the personal nature of hemorrhoids makes seeking treatment away from home a more comfortable and private option.
- High-Quality Care and Facilities: Many medical tourism destinations boast state-of-the-art hospitals, internationally trained surgeons, and excellent patient care standards, often accredited by global bodies.
- Recovery in a Relaxing Environment: Combining your procedure with a stay in a scenic location can transform recovery into a more pleasant, even rejuvenating experience.
Choosing to undergo hemorrhoid removal abroad can be a smart decision for those seeking effective treatment, excellent care, and financial relief.
How can I ensure safety and quality when choosing a clinic for hemorrhoid removal abroad?
The decision to travel for medical care should always prioritize safety and quality. Here's how to ensure you're making an informed and secure choice:
- Accreditation Matters: Look for hospitals and clinics that hold international accreditations, such as Joint Commission International (JCI) or ISO certifications. These indicate adherence to global standards for patient safety and quality of care.
- Surgeon's Qualifications and Experience: Research the surgeon's background. Confirm their board certifications, surgical experience with hemorrhoid removal procedures (especially the one you're considering), and affiliations with reputable medical organizations.
- Facility Standards: Inquire about the modernity of the facility, the technology used, and the hygiene protocols. High-quality clinics will be transparent about their infrastructure.
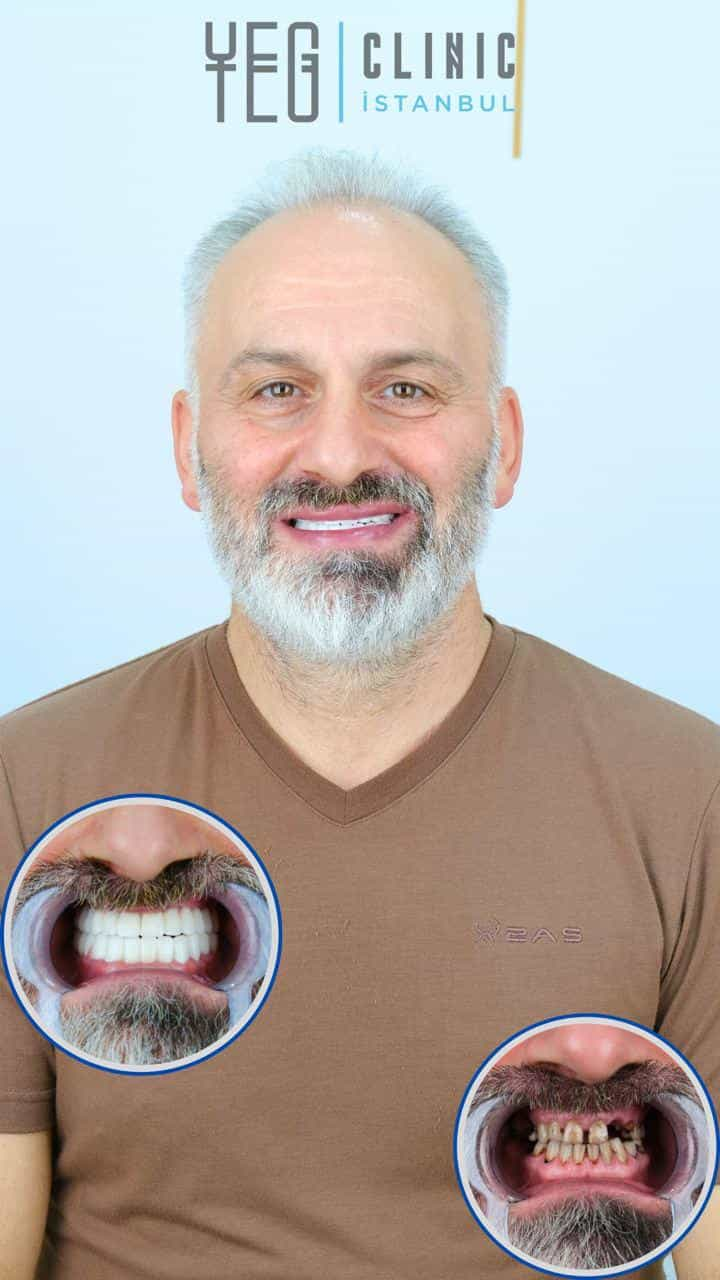
- Patient Reviews and Testimonials: Read reviews from previous international patients. Look for consistent positive feedback regarding care, communication, and outcomes.
- Comprehensive Treatment Plan: Ensure the clinic provides a detailed treatment plan, including pre-operative assessments, the procedure itself, and a clear post-operative care schedule.
- Communication and Language Support: Confirm that there will be clear communication with your medical team. Many international hospitals offer dedicated patient coordinators and interpreters.
- Post-Operative Care and Follow-up: Understand what kind of follow-up care is offered, both while you are abroad and once you return home.
- Medical Tourism Facilitators: Consider working with reputable medical tourism facilitators like PlacidWay. They often vet clinics, streamline the process, and provide a layer of support and advocacy.
Thorough research and asking the right questions are your best tools for a safe and successful medical journey abroad.
What should I expect when traveling abroad for hemorrhoid removal and what are typical patient success stories?
Traveling for medical treatment might seem daunting, but with proper planning, it can be a smooth and rewarding experience. Here's a general overview of what to expect:
- Initial Consultation and Planning: This often starts remotely with your chosen medical tourism provider or clinic. You'll share your medical records, undergo virtual consultations, and receive a personalized treatment plan and cost estimate. Logistics like flights, accommodation, and local transportation may also be arranged.
- Arrival and Pre-operative Appointments: Upon arrival, you'll typically have in-person consultations with your surgeon, undergo any necessary pre-operative tests, and have time to settle in.
- The Procedure and Immediate Recovery: You'll undergo the hemorrhoid removal procedure as planned. Depending on the type of procedure, you might stay in the hospital for a short period or be discharged the same day.
- Post-operative Care and Local Recovery: This is where the medical tourism experience shines. You'll have follow-up appointments, receive pain management, and follow specific recovery instructions. Many patients use this time to recuperate in a comfortable environment, perhaps enjoying light sightseeing or cultural experiences, providing a pleasant distraction from recovery.
- Return Home: Once cleared by your surgeon, you'll travel back home with detailed instructions for continued recovery and follow-up.
Typical Patient Success Stories:
Patients who choose to undergo hemorrhoid removal abroad often share common themes in their success stories:
- Lasting Relief: The most significant outcome is often the profound relief from years of chronic pain, bleeding, and discomfort, leading to a drastically improved quality of life.
- Restored Confidence: Many patients report feeling more comfortable and confident in their daily activities, no longer worried about symptoms or hygiene.
- Exceptional Care at a Fraction of the Cost: Patients frequently express satisfaction with the high level of medical care received, the professionalism of the staff, and the advanced facilities, all while appreciating the substantial cost savings compared to their home countries.
- Smooth Travel and Recovery: With good planning, many find the travel and recovery process surprisingly manageable, often highlighting the support received from their medical tourism facilitator or clinic.
Imagine being able to sit comfortably, use the restroom without dread, and return to your active lifestyle free from the burden of hemorrhoids. For many, hemorrhoid removal abroad makes this a reality, offering not just a procedure, but a renewed sense of well-being.
Take the Next Step with PlacidWay
Ready to explore treatment options abroad? Discover top clinics, compare prices, and get a free quote tailored to your needs with PlacidWay.
Urology Abroad | Best Urology Center








Share this listing