Request a video call
Confirm Your Virtual Consultation
Florence Organ Transplant Center Profile Overview
Comprehensive Transplant Center in Istanbul, Turkey
The transplantation team has performed the highest number of liver transplantations (over 1000) and kidney transplantations (over 750).
As a reference center, the transplantation team performs the most complicated cases and saves hundreds of adult's and children's lives each year.
Group Florence Nightingale Transplantation surgeons have already trained many other colleagues in Turkey, United Kingdom, Romania, Jordan, and India and are proud to serve our patients.
FAQ about Transplant Center in Istanbul, Turkey at Group Florence
What we offer at Group Florence Nightingale Hospitals Comprehensive Transplant Center (CTC)?
- With developed infrastructure facilities and dedicated multidisciplinary teams, Group Florence Nightingale Hospitals Comprehensive Transplantation Center (CTC) is one of the leading reference centers in organ and tissue transplantation (liver, kidney, bone marrow) in Turkey and also for patients from abroad.
- We are discriminated against by performing multiple organ transplantation, such as kidney and liver successfully during the same operation session.
- Group Florence Nightingale CTC is the largest center in Europe for liver, kidney, and pancreas transplantation from living donors.
- As a reference center, the transplantation team performs the most complicated cases and saves hundreds of lives each year. We ensure the recuperation of patients with the gift of life from their relatives via living donors.
- Group Florence Nightingale Transplantation surgeons have already trained many other colleagues in Turkey, United Kingdom, Romania, Jordan, and India and are proud to be at the service of our patients.
Who are Candidates for Organ Transplantation?
The patients with end-stage organ failure are potential candidates for transplantation if,
- their health condition is suitable for a major operation,
- they have donors, who have consented to give part (or one, in case of the kidney) of their functional organs.
How transplantation decision is made for a patient at the CTC?
- If a transplant physician has decided on transplantation, the potential transplant patient is discussed at the CTC board meeting from a multidisciplinary perspective.
- After a comprehensive evaluation of the patient, the final decision for transplant is made at the CTC board meeting.
Who can be a Donor?
Organ donor candidates may be
- Relatives: According to Turkish laws, a person up to the 4th degree of consanguinity, who gives consent, and is suitable, maybe a legal donor for the patient.
- Non-relatives: Potential donors without the 4th degree of consanguinity should be submitted to the Local Ethics Committee of the Health Directorate of the Istanbul City Municipality. Subjects only who gained approval are accepted as donors.
- Cadavers: This option is not available for overseas patients who would like to have transplants in Turkey. Thus, heart transplantation is not legally permitted for foreign patients. Instead left ventricular assist device implantation is provided as the destination treatment.
Liver Transplantation Center in Istanbul, Turkey by Group Florence
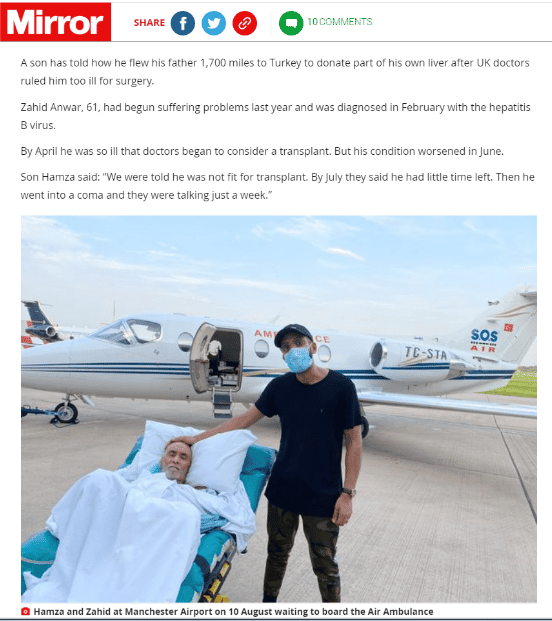
Directed by Prof. Yidiray Yüzer, M.D. the transplant team performs more than 100 transplants per year and has been accomplished more than 1500 transplants since 2004. Each year more than 80% of transplants are being performed from living donors.
Our liver transplant team is the first to perform adult-to-adult right lobe living donor liver transplant, split liver transplant to two adults at the same time, domino liver transplant, and dual left lobe liver transplant.
Based on annual reports of the Turkish Republic, the Ministry of Health, more than 95% of our liver transplant patients are able to live a normal daily life after transplant.
To fulfill our mission of being a pioneering institution that is innovative and continuously improving, we are honored to train not only surgeons but also hepatologists, anesthesiologists, radiologists, intensivists, nurses, coordinators, and technicians from all over Europe.
What do We Offer for our Patients?
- Group Florence Nightingale Hospitals provides healthcare service at international standards. Therefore, it has been entitled to the competency certificate of Joint Commission International (JCI). Our Transplant Center is registered to the European Database of Liver Transplant. The successful outcomes beyond European standards are shared with other European countries on behalf of Turkey.
- Dedicated teamwork in challenging liver conditions: Our transplant team is composed of experienced hepatologists, gastroenterologists, anesthesiologists, radiologists, oncologists, psychiatrists, pathologists, and nurses apart from our distinguished transplant surgeons. After years of close teamwork, they have built up seamless, individualized quality care for each patient and provide high-quality service for diagnosis, treatment and monitoring of any liver diseases.
- Acknowledging that liver transplant is a comprehensive and multidisciplinary procedure, our experts work in collaboration with other specialties for better process management and to improve patient outcomes.
- High-tech facilities. Liver Transplant Center offers advanced technology for diagnosis, treatment, and follow-up of our liver transplant patients. Over 30 years of experience in the healthcare field, Group Florence Nightingale Hospitals has been recognized as a pioneering institution that has closely followed up recent improvements in healthcare technology, and unique contributions in the scientific literature.
Stages of Liver Transplantation Journey
Preparation for the transplant
After a patient is diagnosed as a candidate for transplantation (recipient), it is time to determine a donor (a healthy person who is willing to give a part of his/her liver). Since it is prohibited to have a cadaveric transplant from a Turkish citizen, all of our patients from overseas should have live or swap liver transplants legally.
The recipient (patient) is evaluated for transplantation in 3 stages which will take 5-7 days hospitalization.
Stage 1: Definite diagnosis; determination of liver disease intensity, and emergency of transplant.
Stage 2: Multiple systemic evaluations for transplant such as heart, lungs, kidneys, total blood count. If there is any pathology such as infection, treatment of it. Our experts on the transplant team perform necessary work-ups to estimate transplant success depending on the patient’s condition, underlying cause, and disease intensity.
Stage 3: Psychological and mental preparation of the patient for transplant. The patient and the family members are informed about the procedure, hospitalization, possible progression after surgery, and healthcare issues.
The donor is evaluated for a match with the patient.
Transplantation
From the living donor
In the transplant of the liver from the living donor, the liver part taken from the live donor is transplanted to the recipient immediately after the patient’s liver has been completely removed.
The liver, unlike any other organ in the body, is capable of regeneration and growth making live donor liver transplant possible. The liver's self-feeding starts immediately and lasts for six months. This is why when surgeons remove part of the liver from the donor, the remaining part of the donor and the part placed on the recipient is quickly returned to its original dimensions.
A living donor liver transplant can be performed without waiting for the deceased donor list. Since organ donation is not widespread enough in our country, patients on the list have to wait a long time.
In this process, the patient’s condition may deteriorate, so the rate of success after transplant may decrease as complication risks will increase in the early period after transplant.
Swap Liver Transplant
A swap liver transplant is performed when the blood type of the donor is incompatible with the recipient.
For long years, the organs needed for organ transplantation are obtained from a donor with brain death whose family gives consent or from close relatives who donate a part of their liver. A large number of people in the world has a chance to live and can go back to their active and healthy life through liver transplantation.
Recently, the success rate of liver transplants has rapidly improved with the new drugs and improved surgical techniques, and the postoperative patient survival rate and life of quality have been increased.
Swap liver transplantations, thus, is possible to save many people’s life. Many patients are waiting for the cadaver lists unaware of each other and eventually, die. Our purpose is to bring these people together via our network and enable liver transplants by matching the compatible donors.
After transplantation
The patient is transferred to the intensive care unit (ICU) and is connected to a respiratory assisted device for approximately 26-48 hours. According to his/her general condition, the patient is transferred to the ward. He/she is followed up for fever, jaundice (yellowish coloring of mucosa and skin), pain, fluid accumulation, and transplanted liver functions.
Our patients attend intensive physical and mental rehabilitation programs developed to speed up their recovery.
After discharge from our institution, transplant patients are scheduled for follow-up visits at the outpatient clinic of our center.
Schedule Your Appointment with Group Florence Nightingale in Istanbul, Turkey at PlacidWay!
At PlacidWay, we want to make it easier for you to find the best medical care in Istanbul, Turkey. Our mission is to help you discover the many healthcare options available and provide you with all the necessary tools and resources to make an informed decision. We have partnered with Group Florence Nightingale in Istanbul, Turkey in order to provide you with the highest quality medical care available. Click contact us button below to learn more:
Florence Organ Transplant Center, Istanbul, Turkey Profile Details
Kidney Transplantation Center in Istanbul, Turkey
We are proud to express that we have performed more than 1100 kidney transplantation without any serious health problems at Group Florence Nightingale Hospitals Kidney Transplantation Center.
To have transplantation in Turkey, patients from overseas should have donors up to 4th degree of kinship (Note that spouses are considered to be legal close relatives).
Our Kidney Transplant Center assumes a pioneering role in both pediatric and adult kidney transplant by performing:
- Regular transplant (open surgery),
- Laparoscopic or robotic kidney transplant (closed surgery),
- Kidney transplant under challenging conditions such as cross transplantation, and blood group (ABO) incompatibility.
Benefits of Retroperitoneoscopic Kidney Transplant
With the help of “retroperitoneoscopic” technique, developed by Prof. Baris Akin, MD, the Director of our Kidney Transplant Center, abdominal organs are well-preserved during the operation, so no permanent damage is caused.
At our center, the majority of transplants have been performed by using this technique since 2009. This technique is explained in medical congresses in America, Europe, and Turkey.
- Retroperitoneoscopic technique is a more advanced and secure way “laparoscopic technique”, which is widely performed in the world.
- In laparoscopic technique; the risk of developing damage to intra-abdominal organs, bowel adhesions, and even bowel obstruction during surgery is present due to kidney removal.
- In our center, kidney removal is provided via a small surgical incision under the camera without any contact to intra-abdominal organs using retroperitoneoscopic technique.
- Donors would be discharged 2 or 3 days after the operation.
What about Kidney Transplantation under Challenging Conditions
-
We have a large kidney donor database for patients with kidney failure, who are unable to find eligible donors. By using our donor database and exchanging kidneys between couples, we aim to increase their chances to live with healthy kidneys as well as to help each other for their own good.
-
In nearly 30% of kidney transplantation, patients have donors, but their blood types do not match. In such cases, donors are treated before the surgery, and blood group antigens are nearly cleared out from blood circulation. After that, transplantation is performed. This is called “transplantation between unmatching blood groups” (transplant in ABO blood group incompatibility).
Dedication, scientific knowledge, and accumulated experience lead to higher success rates!
Our kidney transplant team is comprised of:
- Transplant surgeons,
- Nephrologist,
- Anesthesiologist,
- Cardiologist,
- Infectious diseases specialists,
- Immunologist,
- Organ transplant nurses,
- Nephrology assistants,
- Patient coordinators,
- Consultants,
- Other healthcare staff.
Why Choose Us?
As Group Florence Nightingale Kidney Transplant Center, carrying out both scientific and clinical studies with Demiroglu Bilim University, we provide the latest medical technology and apply current advances all through transplantation and for follow-up.
- 99.8% of our patients return home in good health,
- 97.4% of them experience stable good health within the first year of transplantation.
- The success of our kidney transplant team is the same as leading centers in the USA and Europe.
Fundamentals of Group Florence Nightingale Kidney Transplantation Center
- Preventing growth retardation and bone diseases by timely intervention with kidney transplantation in children.
- Thanks to our cross transplantation program to create the chance of transplantation for patients that can receive kidneys from rare people due to blood group in compliance or high antigenic structure.
- Ensuring safe kidney donation by performing an advanced surgical technique under the camera to people to donate their kidney to their relatives (retroperitoneoscopic technique).
- Ensuring healthy work of the kidney for many years with follow-up program after kidney transplantation. Also, follow-up of the people giving their kidneys (donors).
- We collaborate with highly qualified staff from different medical disciplines for the well-being of our patients and donors after transplantation and during follow-up.
- We perform a detailed examination before transplantation so that we can estimate possible immune system reactions after the procedure.
Follow-up after the Kidney Transplant
For successful evaluation of the kidney transplant, follow-up after the kidney transplant as well as the operation period is very important.
At our Kidney Transplant Center, all our patients are followed up closely and regularly to ensure the healthy functioning of the transplanted kidney.
Cornerstones of the calendar after transplant:
- Patients who have received kidneys are discharged after an average of six days.
- Detailed information on the medication and issues requiring special attention in their new life is given 2 days prior to discharge.
- The patient leaves the hospital with a medication chart and a phone number that can be reached 24 hours a day.
- Patients are asked to visit the hospital twice a week to give blood for tests.
- Patients living in distant places may have their blood tests carried out in the regions where they live and sent by mail service without any charges.
- These blood tests are repeated once a week in the second month and once in the sixth month.
- Our patients are regularly asked to visit a Nephrologist.
- We also regularly follow our donors who have given the gift of life to their relatives. Kidney donors can return to their homes within an average of 3 days after the operation.
- They are invited to the hospital for re-examination a week after they return home.
- They come for examinations six months
- Then they are asked to visit the hospital once a year for examination.
Bone Marrow Transplantation Center in Istanbul, Turkey
Directed by Prof. Mutlu Arat, M.D, more than 140 BMTs are being performed annually. Our center is one of 8 project partners with the Turkish Society of Hematology and thus participates also in the scientific areas both nationally and internationally.
Over the years, thousands of patients diagnosed with leukemia, lymphoma, myelodysplasia, multiple myeloma, and other blood cancers or disorders have applied to the Group Florence Nightingale Hospitals BMT Center as one of the most experienced, and well-known transplant center in Europe, and Turkey.
Fundamentals of BMT at the Group Florence Nightingale Hospitals
- Accredited by Joint Accreditation Committee-ISCT & EBMT (JACIE),
- High survival rate within the first year of BMT,
- Long disease-free survival after BMT,
- By the end of the year 2019, 1106 BMTs have performed at our center.
- Life-long follow up program for transplanted patients,
- Center with a dedicated team, high technology, and concrete scientific background,
Our center is not only a healthcare provider but also a training center. We participate in academic events via online training meetings
What is Bone Marrow?
Bone marrow is a spongy material found in the hollow centers of some bones. It is important as it contains special cells known as stem cells.
Stem cells create other specialized cells that carry out important functions. Stem cells in the bone marrow produce three important types of blood cells:
- Red blood cells, which carry oxygen around the body
- White blood cells, which help fight infection
- Platelets, which help stop bleeding
Bone Marrow Transplantation (BMT)
Bone marrow transplantation (also known as stem cell transplantation) involves harvesting healthy stem cells to replenish the bone marrow of the patient. The new stem cells take over the production of the blood cells.
In some circumstances, it may be possible to take your own bone marrow from another part of your body (this is known as autologous transplantation). The bone marrow may be cleared of any diseased cells before being returned.
Stages of BMT Process
There are five stages in the transplant process:
- A physical examination of your body and general state of health
- Obtaining the stem cells that will be used in the transplant (known as harvesting)
- Preparing your body for the transplant (known as conditioning)
- Transplanting the stem cells
- The recovery period, during which you will be monitored for any side effects and complications
Who should have BMT?
Stem cell transplants are normally only recommended if:
- The recipient (the patient who will have transplantation) is in relatively good health, despite the associated condition (which is why stem cell transplants are often done when cancer is in remission)
- Stem cells are available from a brother or sister with the same tissue type, which reduces the chances of the transplant being rejected or graft versus host disease
- The associated condition is not responding to other forms of treatment or it is felt that there is a high risk of the condition returning without a transplant
- It is felt that the benefits of a transplant outweigh the risks.
Florence Organ Transplant Center Certificates, Accreditations, Qualifications Treatments Offered
Best Doctor at Florence Comprehensive Transplant Center in Istanbul, Turkey

Baris AKIN, M.D. Prof.

YUZER, M.D. Prof.

Mutlu ARAT, M.D. Prof.
Heart Transplantation & Cardio-Assisted Devices Center
Unfortunately, we are not allowed to perform heart transplantation in patients who apply from overseas due to local legal issues in Turkey. However, we can help patients with cardiac problems who seek our healthcare by using our highly equipped facilities, such as cardio-assisted devices.
What is heart failure?
Heart failure occurs when the right, left, or both of the ventricles (heart chambers) fail to function. Heart failure is a progressive disease and the power of the heart gradually decreases in time. The heart becomes dysfunctional to pump the required volume of blood by the body. Tissues and cells have difficulty in getting oxygen and nutrients.
Heart failure may occur at any age depending on the underlying cause. However, it occurs in 2.5% of people older than 45 years old and in 10% of those older than 65 years old. End-stage heart failure causes the death of more than half of patients within 1 year of diagnosis.
What are diseases causing heart failure?
-
Coronary Artery Disease: The most common heart disease. Coronary arteries supplying the heart are narrowed and/or obstructed thus the myocardium is unable to get the required oxygen and nutrients and the injured even dies (infarction), resulting in decreased power to contract.
-
Complex Heart Valve Disease: Congenital or acquired aortic and mitral valve disorders increase the workload of the heart, resulting in heart failure due to a dilated or stressed heart.
-
Dilated Cardiomyopathy: The heart is dilated and enlarged leading to heart failure associated with inadequate contraction of the myocardium due to structural defect of the heart muscle.
-
Myocarditis: A disease resulting from decrease power of heart contraction due to a viral infection. Dysfunction of heart contraction might totally disappear after viral infection is healed, or might become permanent, resulting in heart failure.
What is the treatment of heart failure?
Treatment includes:
-
Medications,
-
Diet,
-
Devices to rectify arrhythmia,
-
Corrective surgeries (coronary bypass,
-
Valve surgeries, etc.)
However, the most effective methods in the treatment of end-stage heart failure are heart transplants and support devices for the artificial hearts (cardio-assisted devices).
What is a heart transplant?
A heart transplant is to replace the dysfunctional ill heart with a healthy heart. When a healthy individual dies who donated their organs (donor), their kidneys, liver, heart, etc. are prepared for transplant to patients (receiver) for who a decision to transplant an organ has been previously taken.
Who is a candidate for a heart transplant?
-
Cardiac patients younger than 65 years old are candidates for a heart transplant, who are in end-stage (Stage-D) of heart failure with a life expectancy of less than 1 year.
-
The older patients (65 to 72 years old) are carefully evaluated for their physical characteristics rather than their chronological age and they will be included in the program if they are appropriate.
-
There two common causes for a heart transplant.
-
The first one is coronary artery disease. Such patients are impossible to cure by coronary bypass surgery or balloon-stent procedure. Irreversible myocardial serious or major damage may occur caused by the previous attacks and/or attacks associated with blocked coronary arteries.
-
The second one is congenital or acquired weakness related to bacteria, viruses, etc. of the heart which is called cardiomyopathy. This may require a heart transplant when the contraction power of the myocardium is largely reduced.
-
The other rare causes include rheumatic fever, hypertension, valve diseases resulted in myocardium damage, congenital heart abnormalities impossible to correct surgically, and cardiac tumors
-
Patients with severe arrhythmia are also candidates for a heart transplant.
To be included and voluntarily participate in a heart transplant program, patients and family members should be aware and sure that,
-
All known treatment methods have been considered, applied, and tried for their heart disease,
-
They will lose their life if they do not undergo a heart transplant,
-
They will be able to have the will to adopt the changes in their life and some applications that will be necessary for a lifetime or sometime before, but particularly after the transplant.
-
Patients will be evaluated by specialists in the heart transplant team for the above medical, psychological, and social characteristics to be included in the program.
What is an Artificial Heart Support Device?
An artificial heart support device is a state-of-the-art technology device that assumes the pumping function of the heart in patients with end-stage heart failure. Temporary artificial heart support systems are available used until heart failure is healed, or until a heart transplant as well as permanent artificial heart support systems used for a lifetime.
Who can use Artificial heart support devices?
Heart support devices are used in patients with end-stage heart failure developed instantly or in time for mainly four purposes.
-
For bridging (short-term use) to avoid dysfunctions of other organs in patients who developed instant heart failure and to keep the patient alive until a permanent heart support system is activated.
-
For bridging to recovery to keep the patient alive when the disease shows severe progression, e.g. diseases that lead to sudden heart failure resulting in myocarditis (inflammation of myocardium by viruses, etc.) but are completely healed after a pharmacotherapy.
-
For bridging to heart transplant in patients who are on the waiting list but with a progressed heart failure when waiting for a heart.
-
For use of a lifetime to improve time and quality of life of patients who are unable to have a heart transplant for various reasons (advanced age, severe renal or liver disease, etc.).
How is surgery for artificial heart support devices performed? What happens after the surgery?
Artificial heart support devices are categorized into two groups:
-
Implantable, miniature,
-
Paracorporeal
Which one to the implant will depend on the severity of heart failure and the patient’s general condition.
Although the surgery for artificial heart support devices varies by type of device, it approximately takes 3 to 6 hours. The patients will awaken from anesthesia in an isolated room in the intensive care unit (ICU). By the time, the patient is disconnected from the ventilator (the device helps the patient to breathe).
The patients stay in ICU for 2-3 days after the surgery and then are transferred to the private room where they will stay with a family member.
The duration of the hospital stay is 20-25 days. These patients need to take blood diluents and have periodic blood tests during the whole period they live with a device and consult with their doctor for a dose of the medicines.
Who can have a total artificial heart?
A total artificial heart is a device replaced with the ill heart and implanted in the body.
The first and most used one is Syncardia Cardiowest's total artificial heart to keep the patient alive temporarily, i.e. until the heart is transplanted. It is the latest version of the artificial heart developed by Dr. Kolff and Dr. Jarvik around 50 years ago.
It has been used with a success rate higher than 90% in hundreds of patients. This is the most commonly used total artificial heart.
The other one is the permanent intracorporeal electric motor AbioCor TAH.
Florence Organ Transplant Center Testimonials
Location

About Medical Center
- Translations: EN AR
- Speciality: Organ Transplant, Urology
- Location: Abide-i Hurriyet Cad. No: 166 Sisli - Istanbul , Istanbul , Turkey
- Overview: Florence Comprehensive Organ Transplant Center is to be a pioneering institution that is innovative and constantly improving, offering reliable, up-to-date, and patient-centered healthcare in all services provided, continuously training and educating its staff, and putting patients’ and employees’ welfare at the forefront, as well as respect the environment and patient rights.





.JPG)





.JPG)


.JPG)




.png)








Share this listing