Finding Relief: Your Guide to Percutaneous Vertebroplasty for Spinal Fractures
Are you experiencing persistent back pain that limits your daily activities? Do you suspect a spinal fracture, or has a doctor diagnosed you with a vertebral compression fracture? Living with chronic back pain can be debilitating, affecting your sleep, mobility, and overall quality of life. For many, a procedure called Percutaneous Vertebroplasty (PV) offers a beacon of hope.
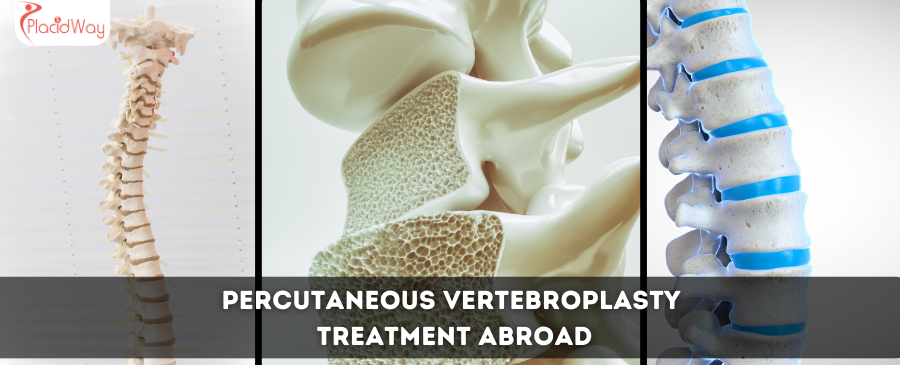
Percutaneous Vertebroplasty is a minimally invasive medical procedure designed to alleviate severe pain caused by vertebral compression fractures (VCFs). These fractures, often a result of osteoporosis, trauma, or certain cancers, cause the bones in your spine (vertebrae) to collapse or crack. During a vertebroplasty, a physician injects medical-grade bone cement into the fractured vertebra, stabilizing it and often providing rapid pain relief. This procedure is a vital option when conservative treatments like bed rest, pain medication, or bracing haven't brought sufficient comfort or healing.
If you're searching for "back pain relief from spinal fracture," "vertebral compression fracture treatment," or "minimally invasive spine procedure," you're in the right place. This guide will walk you through everything you need to know about Percutaneous Vertebroplasty, from understanding its causes and symptoms to exploring treatment options, recovery expectations, and why medical tourism might be a viable and cost-effective path to recovery.
What are the signs of a vertebral compression fracture?
Recognizing the symptoms of a vertebral compression fracture (VCF) is the first step toward seeking appropriate treatment. While some fractures might go unnoticed, many present with clear and often severe signs. If you're wondering "how to know if I have a spinal fracture" or "what does osteoporosis back pain feel like," here are common indicators:
- Sudden, Severe Back Pain: This is the most common symptom. The pain often comes on abruptly, sometimes after a seemingly minor movement like bending, lifting, or even coughing or sneezing. Unlike general backaches, this pain is often sharp and localized to a specific area of the spine.
- Pain Worsens with Movement: The pain typically intensifies when standing, walking, or changing positions. Lying down often brings some relief.
- Limited Mobility: Due to pain, you might find it difficult to bend, twist, or perform everyday activities.
- Loss of Height or Kyphosis (Humped Back): Over time, if multiple vertebrae fracture and collapse, you might notice a decrease in height or the development of a forward curvature of the spine, often referred to as a "dowager's hump."
- Numbness or Tingling (Less Common): While not typical for simple VCFs, if the fracture causes bone fragments to press on spinal nerves, you might experience radiating pain, numbness, or weakness in your limbs. This is more serious and requires immediate medical attention.
- Tenderness: The area over the fractured vertebra may be tender to the touch.
These symptoms can be alarming, prompting many to search for "spinal fracture symptoms" or "pain from collapsed vertebra." If you experience any of these, it's crucial to consult a doctor for an accurate diagnosis, often involving X-rays, MRI, or CT scans.
Why do vertebral compression fractures happen?
Understanding the "causes of spinal fractures" or "why do bones in the spine collapse" is key to prevention and treatment. Vertebral compression fractures (VCFs) occur when the body of a vertebra in the spine collapses. Several factors contribute to this:
- Osteoporosis: This is by far the most common cause, especially in older adults. Osteoporosis causes bones to become porous and brittle, making them fragile and prone to fracture even from minor stresses like bending over, coughing, or simply stepping off a curb. It's often referred to as "brittle bone disease."
- Trauma: High-impact injuries, such as falls, car accidents, or sports injuries, can cause VCFs even in individuals with healthy bones.
- Cancer: Tumors that originate in or spread to the spine (metastatic cancer) can weaken the vertebrae, leading to compression fractures. Myeloma is one such cancer frequently associated with VCFs.
- Benign Tumors: Less commonly, benign tumors within the vertebra can weaken its structure.
- Steroid Use: Long-term use of corticosteroids can weaken bone density, increasing the risk of osteoporosis and subsequent fractures.
- Other Medical Conditions: Conditions like Paget's disease, hyperthyroidism, or osteomalacia can also affect bone strength and contribute to VCFs.
The majority of patients seeking "treatment for osteoporotic fractures" will find their VCFs linked to bone density loss. Awareness of these causes helps in early diagnosis and management.
What types of spinal fracture treatments are available?
When a vertebral compression fracture occurs, physicians typically consider a range of treatment options, often starting with conservative approaches before moving to interventional procedures. Patients researching "how to treat a fractured spine" will encounter these main categories:
Conservative Treatments:
- Rest and Activity Modification: Limiting activities that exacerbate pain, often coupled with temporary bed rest.
- Pain Medication: Over-the-counter pain relievers (like NSAIDs) or prescription medications (such as opioids) to manage pain.
- Bracing: A back brace can help support the spine, reduce movement, and alleviate pain, though long-term use can weaken back muscles.
- Physical Therapy: Once acute pain subsides, exercises to strengthen back muscles and improve posture.
Minimally Invasive Procedures:
If conservative treatments fail to provide adequate pain relief after several weeks or if the pain is severe from the outset, minimally invasive procedures like Vertebroplasty and Kyphoplasty may be recommended. Many search for "vertebroplasty vs kyphoplasty" to understand the differences:
- Percutaneous Vertebroplasty (PV): This procedure involves injecting bone cement (polymethylmethacrylate, or PMMA) directly into the fractured vertebra using a hollow needle guided by X-ray. The cement hardens quickly, stabilizing the bone and significantly reducing pain. It primarily aims for pain relief and stabilization.
- Balloon Kyphoplasty: Similar to vertebroplasty, but before injecting the cement, a balloon is inflated inside the collapsed vertebra to help restore some of its original height. The balloon is then deflated and removed, creating a cavity that is then filled with bone cement. Kyphoplasty not only stabilizes the bone and relieves pain but can also correct some spinal deformity and restore vertebral height, potentially preventing further height loss or kyphosis.
Both procedures are typically performed under local anesthesia with sedation, are relatively quick, and offer substantial pain relief for suitable candidates. Your doctor will determine which approach is best based on your specific fracture and overall health.
Am I a good candidate for vertebroplasty?
Determining "who is eligible for vertebroplasty" or "when is vertebroplasty recommended" is crucial. Not everyone with a spinal fracture is an ideal candidate. Physicians consider several factors:
- Persistent Pain: The most significant factor is severe, disabling back pain directly attributable to a vertebral compression fracture that has not responded to conservative treatments (rest, pain medication, bracing) after 2-4 weeks.
- Recent Fracture: Vertebroplasty is most effective for acute or subacute fractures, typically less than 2-3 months old. Older, well-healed fractures may not benefit as much from stabilization.
- Imaging Confirmation: An MRI or bone scan should confirm the fracture is recent and painful (active). X-rays alone may not provide enough detail about fracture age.
- Stable Neurological Status: Patients with no evidence of spinal cord compression or nerve damage from the fracture itself are typically better candidates. If there's neurological compromise, surgery might be a more appropriate option.
- Good General Health: Patients should be healthy enough to undergo a minimally invasive procedure, usually under local anesthesia and sedation. Significant bleeding disorders or active infections might contraindicate the procedure.
- No Significant Vertebral Instability: If the fracture is severely unstable or involves significant loss of vertebral body height, kyphoplasty (which attempts to restore height) or more extensive open surgery might be considered instead.
A thorough evaluation by a spine specialist, including physical examination and imaging studies, is essential to determine if Percutaneous Vertebroplasty is the right choice for your condition. If you're searching for "is vertebroplasty right for me?", a consultation is the best next step.
What is the recovery time after vertebroplasty?
One of the appealing aspects of Percutaneous Vertebroplasty is its relatively quick recovery time compared to traditional open spine surgery. Patients often look for "vertebroplasty recovery timeline" or "how quickly will I feel better after vertebroplasty."
- Immediate Post-Procedure: Patients typically spend a few hours recovering in the hospital or clinic after the procedure, usually lying flat to allow the cement to fully harden and to monitor for any immediate complications.
- Within 24-48 Hours: Many patients report significant pain relief within this timeframe. You may be able to walk and perform light daily activities. Some soreness at the injection site is common.
- First Few Days: You'll likely be advised to avoid heavy lifting and strenuous activities for a few days to a week. Pain medication may be prescribed to manage any residual discomfort.
- Within 1-2 Weeks: Most patients can gradually return to their normal, non-strenuous activities. Your doctor may recommend a walking program to improve mobility and strength.
- Full Recovery: While pain relief is often immediate, full recovery and strength building may take several weeks. Physical therapy might be suggested to help rebuild strength and flexibility, especially if you had prolonged inactivity due to pain.
It's important to follow your doctor's specific post-operative instructions, as individual recovery can vary based on your overall health, the severity of the fracture, and how long you've been experiencing pain.
What are the risks of vertebroplasty?
Like any medical procedure, Percutaneous Vertebroplasty carries potential risks and side effects, though they are generally low. Patients often search for "is vertebroplasty safe?" or "vertebroplasty complications." Here are the main concerns:
- Cement Leakage: This is the most common risk. If the bone cement leaks out of the fractured vertebra, it can potentially irritate or compress nearby nerves or the spinal cord, leading to pain, numbness, weakness, or in rare cases, paralysis. It can also leak into blood vessels, potentially reaching the lungs (pulmonary embolism), though this is very rare.
- Infection: As with any invasive procedure, there's a small risk of infection at the injection site or within the spine.
- Bleeding: Minor bleeding or bruising at the needle insertion site is possible.
- Allergic Reaction: To anesthesia, contrast dye, or the bone cement components.
- Rib or Adjacent Vertebra Fracture: The pressure of the needle or cement injection can, in rare instances, cause a new fracture in a nearby bone.
- Increased Pain: While rare, some patients may experience temporary or increased pain following the procedure, or the pain may not improve.
- Lung Issues: In extremely rare cases, cement leakage into the lung arteries can cause shortness of breath or chest pain.
The risk of serious complications is low (estimated to be less than 1-2%). An experienced surgeon performing the procedure under image guidance significantly minimizes these risks. Always discuss your specific risk factors and concerns with your doctor.
Worldwide Cost Comparison for Percutaneous Vertebroplasty
For many patients, especially those without comprehensive insurance or facing high deductibles, the "cost of vertebroplasty" can be a major factor. This is where medical tourism often presents a compelling alternative. Prices for Percutaneous Vertebroplasty can vary widely depending on the country, clinic, surgeon's experience, and what's included in the package (e.g., hospital stay, anesthesia, follow-up). Here's an estimated cost comparison:
| Country | Estimated Cost (USD) | Notes |
|---|---|---|
| United States | $8,000 - $15,000+ | High costs, often dependent on insurance coverage and facility fees. |
| Canada | $7,000 - $12,000 | Generally covered by public healthcare, but private costs can be high for non-residents. |
| United Kingdom | £5,000 - £9,000 ($6,000 - $11,000) | NHS may have waiting lists; private treatment is comparable to US. |
| Mexico | $2,500 - $5,000 | Popular for US patients due to proximity and significant savings. |
| India | $2,000 - $4,500 | Known for advanced medical facilities and highly competitive prices. |
| Turkey | $3,000 - $6,000 | Growing medical tourism hub with modern hospitals and experienced doctors. |
| Costa Rica | $3,500 - $7,000 | Offers high-quality care at a fraction of Western costs, popular for US and Canadian patients. |
| Poland | $2,800 - $5,500 | Emerging destination in Eastern Europe with good standards and lower costs. |
*Costs are estimates and can vary based on the specific clinic, surgeon, and inclusions. Always request a detailed quote.
The significant cost disparity often drives patients to explore "vertebroplasty abroad" options, ensuring access to quality care without financial strain.
Why consider vertebroplasty abroad?
Many patients are increasingly looking into "medical tourism for spinal treatment" or "affordable vertebroplasty overseas." Here’s why:
- Significant Cost Savings: As seen in the table above, the cost of vertebroplasty in countries like India, Mexico, or Turkey can be 50-70% lower than in Western nations, even when factoring in travel and accommodation.
- Access to Timely Treatment: In some countries, public healthcare systems may have long waiting lists for elective procedures, delaying crucial pain relief. Medical tourism allows for prompt scheduling.
- High-Quality Care: Many international clinics and hospitals catering to medical tourists are accredited by international bodies (like JCI) and boast state-of-the-art technology and highly qualified, often internationally trained, medical professionals.
- Privacy and Anonymity: For some, undergoing treatment away from home offers a sense of privacy.
- Recovery in a Relaxing Environment: Combining a medical procedure with a stay in a new country can make the recovery process feel less clinical and more like a rejuvenating retreat.
The decision to travel for medical care is personal, but the benefits of cost-effectiveness, quality, and accessibility make it a compelling choice for many seeking "spine care abroad."
Which countries offer the best value for vertebroplasty?
When searching for "best countries for vertebroplasty" or "top medical tourism destinations for spine surgery," several nations stand out due to their blend of affordability, quality, and infrastructure:
- Mexico: Especially popular for North American patients due to its close proximity, Mexico offers modern hospitals and clinics with U.S.-trained physicians at a significantly lower cost. Cities like Tijuana, Cancun, and Guadalajara are medical tourism hotspots.
- India: A global leader in medical tourism, India provides world-class healthcare facilities, highly skilled spine specialists, and exceptionally competitive pricing for vertebroplasty. English is widely spoken in medical settings.
- Turkey: With its strategic location, state-of-the-art hospitals, and skilled medical professionals, Turkey has become a fast-growing destination for various medical procedures, including spine treatments.
- Costa Rica: Known for its beautiful scenery and excellent patient care, Costa Rica offers high-quality medical services at more affordable rates, particularly attractive to those from North America.
- Poland: An emerging destination in Europe, Poland offers modern clinics, well-trained doctors, and competitive prices, making it a viable option for European patients seeking value.
These countries have established medical tourism sectors, making the process relatively smooth for international patients. They prioritize patient safety and satisfaction, making them reliable choices for "international vertebroplasty."
What to expect when traveling for vertebroplasty?
Embarking on a medical journey abroad can feel daunting, but with proper planning, it's a smooth process. If you're wondering "how to plan medical travel for spine treatment" or "what's involved in overseas medical care," here's a general outline:
- Initial Consultation & Planning: Start with a virtual consultation with an international specialist. Share your medical records, imaging (X-rays, MRI), and diagnosis. The clinic will provide a treatment plan and cost estimate.
- Travel Arrangements: Once you decide, book your flights and accommodation. Many medical tourism agencies (like PlacidWay) offer assistance with this, including airport transfers and local logistics.
- Pre-operative Tests Abroad: Upon arrival, you'll undergo a physical examination and any necessary pre-operative tests (blood work, additional imaging) to ensure you are fit for the procedure.
- The Procedure: Vertebroplasty is typically an outpatient or overnight stay procedure. You'll usually be under local anesthesia and sedation.
- Recovery Period: A short recovery stay is needed, often a few days to a week, allowing for follow-up appointments and ensuring stable recovery before flying home.
- Post-operative Care & Follow-up: The clinic will provide detailed instructions for your post-operative care. Many offer virtual follow-ups once you return home.
Choosing a reputable medical tourism facilitator can greatly simplify these steps, offering peace of mind and handling many of the logistical challenges.
How to ensure safety and quality for vertebroplasty abroad?
Safety and quality are paramount when considering "safe vertebroplasty overseas" or "choosing a reputable international clinic." Here's how to ensure you're making an informed decision:
- Accreditation: Look for hospitals and clinics accredited by international organizations like the Joint Commission International (JCI). This signifies adherence to rigorous quality and patient safety standards.
- Surgeon Credentials: Verify the qualifications, experience, and specialization of the spine surgeon. Many international doctors have received training in Western countries. Ask about their success rates with vertebroplasty.
- Facility Standards: Research the clinic's technology, cleanliness, and infrastructure. Websites, virtual tours, and patient testimonials can provide insights.
- Patient Reviews and Testimonials: Read reviews from previous international patients. Look for consistent positive feedback regarding care, results, and overall experience.
- Transparent Communication: Ensure clear and direct communication with the clinic and your medical coordinator. They should be able to answer all your questions thoroughly and in a language you understand.
- Medical Tourism Facilitators: Partner with a reputable company like PlacidWay. They vet clinics, manage logistics, and act as an advocate for your needs, providing an extra layer of safety and support.
- Comprehensive Package: Ensure the treatment package includes all necessary costs (pre-op, procedure, post-op, medications, hospital stay) to avoid hidden fees.
By taking these steps, you can significantly mitigate risks and enhance your chances of a successful and safe "spine fracture treatment abroad."
What are patient success stories from vertebroplasty abroad?
Hearing about real-world experiences can be incredibly reassuring when considering "vertebroplasty success rates" or "patient testimonials for spine surgery abroad." Many patients who have traveled for vertebroplasty share similar positive outcomes:
- Rapid Pain Relief: A common theme is the quick resolution of debilitating back pain, often within days of the procedure. Patients describe going from severe, constant pain to mild discomfort or no pain at all.
- Return to Mobility: With pain significantly reduced, patients report being able to walk, sit, and move much more freely than before. This restoration of mobility is life-changing for many who were previously sedentary due to pain.
- Improved Quality of Life: Beyond just pain relief, success stories often emphasize a significant improvement in overall quality of life. Patients can return to hobbies, spend time with family, and perform daily tasks without the constant burden of pain.
- Positive Medical Tourism Experience: Many patients praise the high standard of care, the professionalism of the medical staff, and the efficiency of the international clinics. They often feel well-supported throughout their journey, from initial inquiry to post-operative follow-up.
- Affordability Without Compromise: Patients frequently express satisfaction with the cost savings, noting that they received excellent medical care without having to deplete their savings or go into debt.
These stories reinforce that high-quality, effective vertebroplasty is not only achievable abroad but often comes with added benefits of affordability and a positive patient experience, empowering patients to take control of their health.
Take the Next Step with PlacidWay
Ready to explore treatment options abroad? Discover top clinics, compare prices, and get a free quote tailored to your needs with PlacidWay.
Orthopedic Surgery Abroad, Knee Sugery Abroad








Share this listing