Navigating Shunt Procedure: Your Guide to Hydrocephalus Treatment & Medical Travel
Facing a diagnosis that may require a shunt procedure can bring a mix of emotions – from concern about your health to questions about the best path forward. For many, a shunt procedure is a life-changing intervention, offering relief from the debilitating symptoms caused by excess fluid buildup in the brain, most commonly known as hydrocephalus. Understanding this delicate neurosurgical procedure is the first step towards recovery and regaining your quality of life.
A shunt acts like a sophisticated drainage system for your brain. When the delicate balance of cerebrospinal fluid (CSF) production and absorption is disrupted, pressure can build up, leading to a host of neurological issues. The shunt, a thin, flexible tube with a one-way valve, is surgically placed to divert this excess fluid to another area of the body, typically the abdomen, where it can be safely reabsorbed. This procedure is crucial for managing conditions like hydrocephalus, improving symptoms, and preventing further brain damage.
Whether you're exploring options for yourself or a loved one, this comprehensive guide will walk you through everything you need to know about shunt procedures, from recognizing the symptoms that necessitate it to understanding the recovery process and considering the benefits of medical tourism for this specialized treatment. We'll delve into the types of shunts, potential risks, and a crucial aspect for many – the cost comparisons worldwide. Our goal is to empower you with knowledge, helping you make informed decisions about your healthcare journey, even if it means looking beyond your local borders for the best possible care.
What Are the Common Symptoms That Might Suggest a Shunt Is Needed?
Recognizing the signs and symptoms of conditions like hydrocephalus is crucial for early diagnosis and treatment. These symptoms can vary depending on age, the rate of fluid buildup, and the underlying cause. If you or a loved one are experiencing several of these, it's vital to seek medical attention promptly. Common indicators include:
- Headaches: Often persistent, worsening with activity, and relieved by lying down.
- Nausea and Vomiting: Especially in the morning, sometimes without headache.
- Vision Problems: Blurry vision, double vision, or difficulty focusing.
- Balance and Coordination Issues: Gait disturbances, frequent falls, or unsteadiness.
- Cognitive Decline: Memory loss, difficulty concentrating, confusion, or changes in personality (common in Normal Pressure Hydrocephalus, or NPH).
- Fatigue and Drowsiness: Increased sleepiness or difficulty staying awake.
- In Infants: An unusually large head circumference, a bulging soft spot (fontanelle), irritability, poor feeding, or downward-gazing eyes (sunsetting eyes).
- In Children: Delayed development, behavioral changes, or problems with school performance.
These symptoms are the brain's cry for help, signaling that the pressure from excess cerebrospinal fluid is interfering with its normal function. Don't ignore them; early intervention with a shunt procedure can significantly improve outcomes.
What Causes Hydrocephalus and What Are Its Risk Factors?
Hydrocephalus, the primary condition treated by shunt procedures, arises from a disruption in the delicate system that manages cerebrospinal fluid (CSF) around the brain and spinal cord. Think of CSF as the brain's protective cushion and waste removal system. When its flow is obstructed, its absorption is impaired, or it's overproduced, pressure builds up. The causes and risk factors are diverse:
- Congenital Hydrocephalus: Present at birth, often due to developmental problems like aqueductal stenosis (narrowing of the aqueduct of Sylvius), spina bifida, or other brain malformations.
- Acquired Hydrocephalus: Develops after birth due to various factors:
- Brain Hemorrhages: Bleeding in the brain (e.g., from a stroke, aneurysm, or head trauma) can block CSF pathways.
- Infections: Meningitis or encephalitis can cause inflammation that obstructs CSF flow.
- Brain Tumors: Tumors can directly block CSF pathways or interfere with absorption.
- Head Injuries: Severe head trauma can lead to swelling, bleeding, or scarring that impedes CSF circulation.
- Normal Pressure Hydrocephalus (NPH): Often affects older adults, characterized by enlarged ventricles but with CSF pressure that appears normal during a spinal tap. The cause is often unknown, but it can be linked to prior head injury, stroke, or infection.
Understanding the root cause helps doctors determine the most appropriate type of shunt and treatment plan, making it essential to have a thorough diagnostic evaluation.
What Are the Different Types of Shunt Procedures for Hydrocephalus?
Shunts are categorized by where the CSF is drained from and to. Each type is designed to address specific needs and anatomical considerations:
- Ventriculoperitoneal (VP) Shunt: This is the most common type. The shunt tubing is placed in one of the brain's ventricles, tunnels under the skin, and drains the CSF into the peritoneal cavity (the space in the abdomen containing the digestive organs). The peritoneum can absorb the excess CSF effectively.
- Ventriculoatrial (VA) Shunt: Less common today due to potential cardiac complications, this shunt drains CSF from a brain ventricle into a chamber of the heart (the right atrium). It's typically considered when a VP shunt is not feasible.
- Lumboperitoneal (LP) Shunt: This shunt drains CSF from the lumbar spine (lower back) into the peritoneal cavity. It's often used for conditions where the hydrocephalus is primarily a problem of CSF absorption in the spinal fluid space, such as idiopathic intracranial hypertension or sometimes in certain types of communicating hydrocephalus.
- Ventriculopleural (VPL) Shunt: Rarely used, this drains CSF into the pleural cavity (the space surrounding the lungs). It's typically reserved for cases where other shunt types are not an option.
All shunt systems include a catheter placed in the CSF space, a one-way valve to regulate pressure and flow, and a distal catheter to drain the fluid. The choice of shunt type is determined by a neurosurgeon based on the patient's specific condition and medical history.
Who Is a Candidate for a Brain Shunt Procedure?
Not everyone with excess CSF needs a shunt, but certain criteria help identify ideal candidates. Generally, a shunt procedure is considered for individuals diagnosed with hydrocephalus who are experiencing symptoms severe enough to impact their quality of life or pose a risk to their neurological health. This includes:
- Individuals with Communicating Hydrocephalus: Where CSF flow is not blocked, but absorption is impaired.
- Individuals with Non-Communicating Hydrocephalus: Where CSF flow is obstructed within the brain's ventricular system.
- Patients with Normal Pressure Hydrocephalus (NPH): Especially those who show improvement after a diagnostic CSF tap test.
- Infants and Children: Born with congenital hydrocephalus or who develop it due to infections or bleeding.
- Adults: Who develop hydrocephalus secondary to brain tumors, trauma, stroke, or infection.
Eligibility is determined by a thorough neurological examination, imaging studies (MRI, CT scans), and sometimes CSF flow studies. A multidisciplinary team evaluates the benefits versus the risks, considering the patient's overall health and the specific nature of their hydrocephalus.
What Is the Recovery Process Like After Shunt Surgery and What Should I Expect?
Recovery from a shunt procedure varies among individuals, but there are general expectations. Immediately after surgery, patients are closely monitored in the hospital for a few days.
- Hospital Stay: Typically 3-7 days, depending on the patient's condition and the specific procedure. Pain management is crucial, and patients are monitored for signs of infection or shunt malfunction.
- Initial Recovery (First few weeks): Patients may experience fatigue, headaches, or some discomfort at the incision sites (on the head and abdomen). Light activities are usually permissible, but strenuous exercise, heavy lifting, and contact sports are restricted.
- Long-Term Recovery (Weeks to Months): Most individuals gradually return to their normal daily routines. It's common to have follow-up appointments with the neurosurgeon to check shunt function and adjust valve settings if the shunt is programmable. Regular imaging scans may be done to monitor CSF levels.
- Lifestyle Adjustments: While most patients lead normal lives, awareness of the shunt is important. Avoiding direct impacts to the shunt site and being mindful of symptoms that could indicate a malfunction are key.
The goal of recovery is not just physical healing but also the improvement of hydrocephalus symptoms. Patience and adherence to medical advice are crucial for a successful outcome.
What Are the Potential Risks and Side Effects of a Shunt Procedure?
Like any surgical procedure, shunt placement comes with potential risks and side effects, although serious complications are rare. It's important to discuss these with your medical team:
- Infection: This is the most common complication and can occur at any point along the shunt system. Symptoms include fever, redness/swelling along the shunt path, and headaches. Infections often require antibiotics and potentially shunt removal and replacement.
- Shunt Malfunction: Shunts can become blocked (e.g., by tissue or blood) or break, leading to a return of hydrocephalus symptoms. Malfunctions often require further surgery to revise or replace the shunt.
- Over-drainage: The shunt drains too much CSF too quickly, leading to symptoms like severe headaches (especially when upright), nausea, vomiting, or even a subdural hematoma (blood clot outside the brain).
- Under-drainage: The shunt doesn't drain enough CSF, causing symptoms of hydrocephalus to persist or worsen.
- Bleeding: Hemorrhage can occur during or after surgery, potentially leading to neurological complications.
- Seizures: While rare, seizures can sometimes be a complication of brain surgery.
- Other Risks: include scarring, pain at incision sites, abdominal problems (for VP shunts), and less commonly, neurological deficits.
Constant monitoring and regular follow-up are vital to catch and address any potential complications early.
How Much Does a Shunt Procedure Cost Worldwide, and What Factors Influence It?
The cost of a shunt procedure can be a major concern for patients and their families, often leading them to explore international options. Prices can vary dramatically based on location, healthcare system, and included services.
Worldwide Shunt Procedure Cost Comparison (Estimated)
| Country | Estimated Cost Range (USD) | Typical Inclusions |
|---|---|---|
| United States | $50,000 - $150,000+ | Hospital fees, surgeon fees, anesthesia, standard pre/post-op care, some device costs. |
| United Kingdom | $40,000 - $80,000+ | Similar to US, often slightly lower for private care. |
| India | $10,000 - $25,000 | Surgery, hospital stay, medications, basic diagnostics. Travel and accommodation extra. |
| Turkey | $12,000 - $30,000 | Surgery, hospital stay, some pre-op tests, initial follow-up. |
| Mexico | $15,000 - $35,000 | Surgery, hospital stay, surgeon's fees. Often popular for US patients seeking value. |
| Thailand | $15,000 - $35,000 | Comprehensive packages common, including hospital, surgeon, basic post-op. |
Factors influencing cost:
- Country & Healthcare System: Countries with lower living costs and different healthcare economic models can offer significant savings.
- Hospital Accreditation & Reputation: Highly specialized, internationally accredited hospitals often charge more but offer advanced technology and expertise.
- Surgeon's Experience: Renowned neurosurgeons with extensive experience may command higher fees.
- Type of Shunt: Programmable shunts, which allow external adjustment of CSF flow, can be more expensive than fixed-pressure shunts.
- Length of Hospital Stay: Longer stays due to complications or recovery time increase costs.
- Inclusions: Some packages include pre-operative tests, medications, follow-up consultations, and even accommodation, while others only cover the surgery itself.
Why Consider Medical Tourism for a Shunt Procedure Abroad?
For many patients, looking beyond their national borders for a shunt procedure isn't just an option—it's a necessity or a strategic choice. Here's why medical tourism is increasingly popular for complex neurosurgical procedures:
- Significant Cost Savings: As seen in the table above, the cost difference for a shunt procedure can be staggering. Patients can save anywhere from 50% to 80% compared to prices in Western countries, even when factoring in travel and accommodation.
- Access to Advanced Care and Specialized Surgeons: Many international hospitals boast state-of-the-art facilities, cutting-edge technology, and neurosurgeons with extensive experience in shunt procedures, often trained in leading global institutions.
- Reduced Wait Times: In some countries, healthcare systems can have long waiting lists for specialized surgeries. Medical tourism offers the ability to schedule and receive treatment much faster.
- Privacy and Anonymity: For some, the privacy offered by receiving treatment away from home is a significant draw.
- A Chance for a "Medical Vacation": While recovery is the priority, combining treatment with an opportunity to recover in a pleasant, often tourist-friendly environment can enhance the overall experience.
Choosing to travel for a shunt procedure allows patients to find a balance between high-quality medical care and financial practicality, opening doors to life-changing treatment that might otherwise be out of reach.
Which Countries Offer the Best Value for Shunt Surgery and Hydrocephalus Treatment?
When seeking the "best value," patients are looking for a combination of affordability, quality, and accessibility. Several countries have established themselves as leaders in medical tourism for neurosurgical procedures, including shunt placement:
- India: Known for its highly skilled neurosurgeons, advanced medical technology, and some of the most competitive prices globally. Many hospitals are internationally accredited (JCI) and cater specifically to international patients.
- Turkey: Offers a modern healthcare system with many JCI-accredited hospitals, particularly in cities like Istanbul. It provides high-quality care at a fraction of Western costs, often with comprehensive medical tourism packages.
- Mexico: A popular choice for North American patients due to geographical proximity. Mexican hospitals, especially in border cities and major hubs like Mexico City, offer state-of-the-art facilities and experienced neurosurgeons at attractive prices.
- Thailand: A long-standing leader in medical tourism, Thailand boasts world-class hospitals, highly trained medical staff, and excellent patient care services, all within a vibrant cultural setting.
- Malaysia and South Korea: Also emerging as strong contenders, offering advanced medical technology and excellent patient outcomes, often with a focus on personalized care.
These countries not only provide cost-effective treatment but also often include comprehensive services such as airport transfers, language support, and accommodation assistance, making the medical journey smoother for international patients.
What Should I Expect When Traveling Abroad for a Shunt Procedure?
Undertaking a medical journey to another country requires careful preparation. Here’s a general outline of what to expect:
- Initial Consultation & Planning: Start by contacting a medical tourism facilitator or the international patient department of your chosen hospital. They will review your medical records, provide a treatment plan, and an estimated cost. This is often done remotely via telemedicine.
- Travel Arrangements: Book flights, accommodation (often near the hospital for convenience during recovery), and transportation. Many medical tourism providers assist with these logistics.
- Visa & Documentation: Ensure you have the necessary visas and all medical documents translated into English (or the local language, if required).
- Arrival & Pre-operative Assessments: Upon arrival, you'll undergo thorough pre-operative tests, consultations with the neurosurgeon and anesthesiologist, and any necessary imaging.
- The Procedure & Hospital Stay: After the shunt procedure, you'll have a hospital stay (typically 3-7 days) for initial recovery and monitoring.
- Post-operative Recovery & Follow-up: You'll need to stay in the country for a period after discharge, usually 1-3 weeks, for outpatient follow-up appointments, wound care, and to ensure stable recovery before flying home. This is crucial for shunt procedures due to the need for monitoring for complications.
- Language & Cultural Differences: Most international hospitals catering to medical tourists have English-speaking staff and translators. Be prepared for cultural differences but expect a high level of hospitality.
A well-planned trip minimizes stress and allows you to focus solely on your recovery.
How to Ensure Safety and Quality When Getting a Shunt Placement Abroad?
The decision to undergo a complex procedure like shunt placement abroad should always prioritize safety and quality. Here’s how you can ensure you're making the best choice:
- Choose Internationally Accredited Hospitals: Look for hospitals with international accreditations like Joint Commission International (JCI). JCI accreditation signifies that a hospital meets stringent global healthcare quality and patient safety standards.
- Verify Neurosurgeon Credentials: Research the surgeon's qualifications, experience, and specialization in shunt procedures. Many top surgeons in medical tourism destinations have international training and board certifications.
- Review Patient Testimonials and Outcomes: Look for reviews and testimonials from other international patients who have undergone similar procedures. Ask for data on success rates and complication rates if available.
- Use Reputable Medical Tourism Facilitators: Organizations like PlacidWay specialize in connecting patients with vetted, high-quality international providers. They can offer guidance, logistical support, and ensure you're dealing with legitimate and safe options.
- Communicate Clearly: Ensure there are clear communication channels with your medical team before, during, and after your trip. Language support is crucial.
- Understand the Entire Package: Be clear on what is included in the cost – does it cover pre-op, surgery, hospital stay, medications, follow-up, and any potential complications?
- Consider Travel Insurance: Purchase comprehensive medical travel insurance that covers emergency evacuation or extended stays if unexpected complications arise.
Due diligence is paramount. By researching thoroughly and asking the right questions, you can confidently pursue quality care overseas.
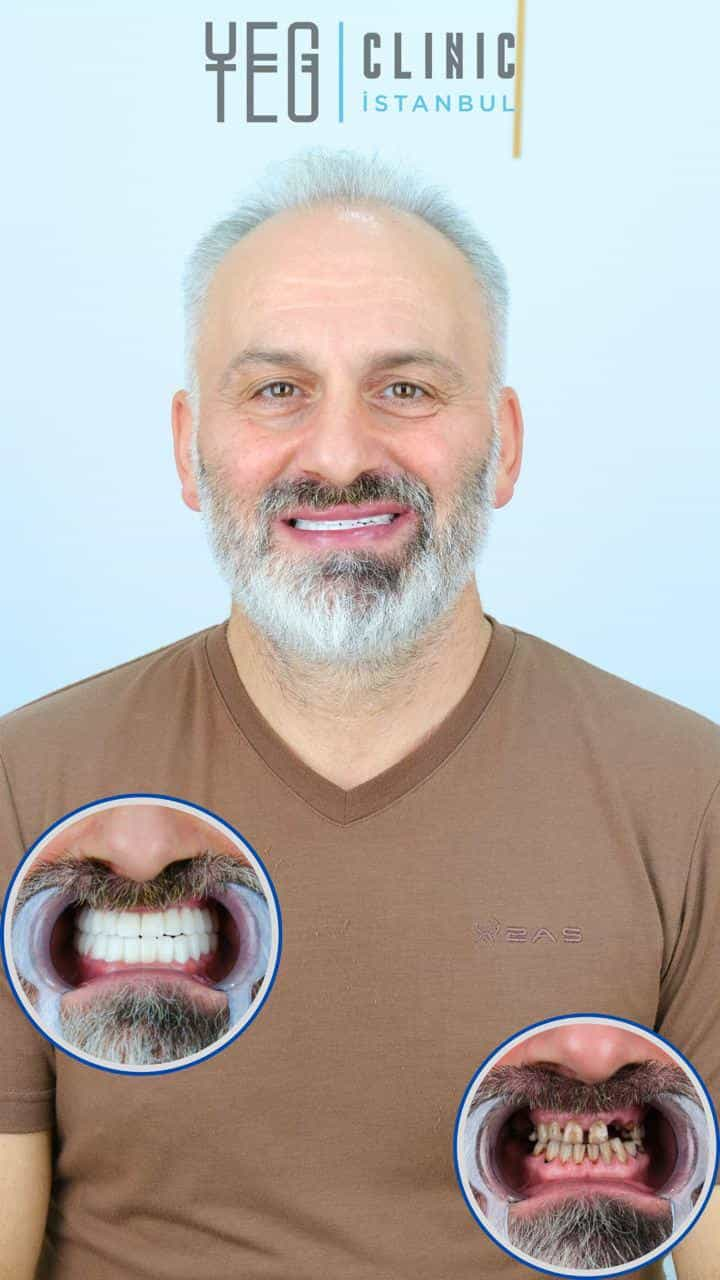
What Are Patient Success Stories Like for Shunt Procedures from Abroad?
Patient success stories are powerful indicators of the quality and effectiveness of medical tourism. For shunt procedures, these stories often echo similar themes:
- Life-Changing Relief: Patients frequently describe a dramatic improvement in symptoms like chronic headaches, balance issues, and cognitive fog. "I got my life back," is a common sentiment. For children, parents often report improvements in development and overall well-being.
- Affordability Without Compromise: Many patients share how they received world-class treatment from highly skilled neurosurgeons at a fraction of the cost they would have paid at home, making critical surgery accessible.
- Exceptional Patient Care: Testimonials often highlight the personalized attention, compassionate nursing staff, and comprehensive support services provided by international hospitals, often exceeding expectations.
- Smooth Travel Experience: Patients frequently commend medical tourism facilitators and hospital international departments for handling logistics seamlessly, from airport transfers to accommodation and translation services, reducing the stress of traveling for surgery.
- Renewed Hope: For individuals facing long wait times or prohibitive costs in their home countries, successful shunt surgery abroad provides renewed hope and a fresh start.
These real-world examples underscore the potential of medical tourism to deliver both excellent medical outcomes and a positive overall experience for those needing a shunt procedure. Always seek reputable sources and verified testimonials for accurate insights.
Take the Next Step with PlacidWay
Ready to explore treatment options abroad? Discover top clinics, compare prices, and get a free quote tailored to your needs with PlacidWay.
Affordable Spine Surgery | Best Spine Surgery Abroad







Share this listing