A Guide to Gene Therapy for Thalassemia

If you or a loved one is living with thalassemia, you know it's a lifelong journey. This inherited blood disorder, which affects the body's ability to produce hemoglobin, often means a routine of frequent blood transfusions and chelation therapy just to manage the symptoms. For decades, the only potential cure has been a bone marrow transplant, which comes with its own set of significant risks and reliance on a suitable donor. But what if there was another way? What if you could fix the genetic "typo" at its source?
This is where the groundbreaking science of gene therapy steps in. The buzz around this topic is undeniable, and for good reason. We're moving from an era of managing a chronic illness to potentially offering a one-time, permanent thalassemia cure. It's a concept that brings immense hope, but it also brings a lot of questions. Is it safe? Does it really work? How much does it cost? And who is it for?
You're not alone in asking these questions. People all over the world are searching for clear, trustworthy information on gene therapy for thalassemia. That's why we've created this comprehensive guide. We'll break down everything you need to know, answering the most common and critical questions about this revolutionary treatment, so you can feel informed and empowered.
What exactly is gene therapy for thalassemia?
Think of your DNA as a giant instruction manual for your body. In thalassemia, there's a critical error—a "typo"—in the instructions for making hemoglobin, the protein in red blood cells that carries oxygen. Because of this error, your body either doesn't make enough hemoglobin or makes a faulty version.
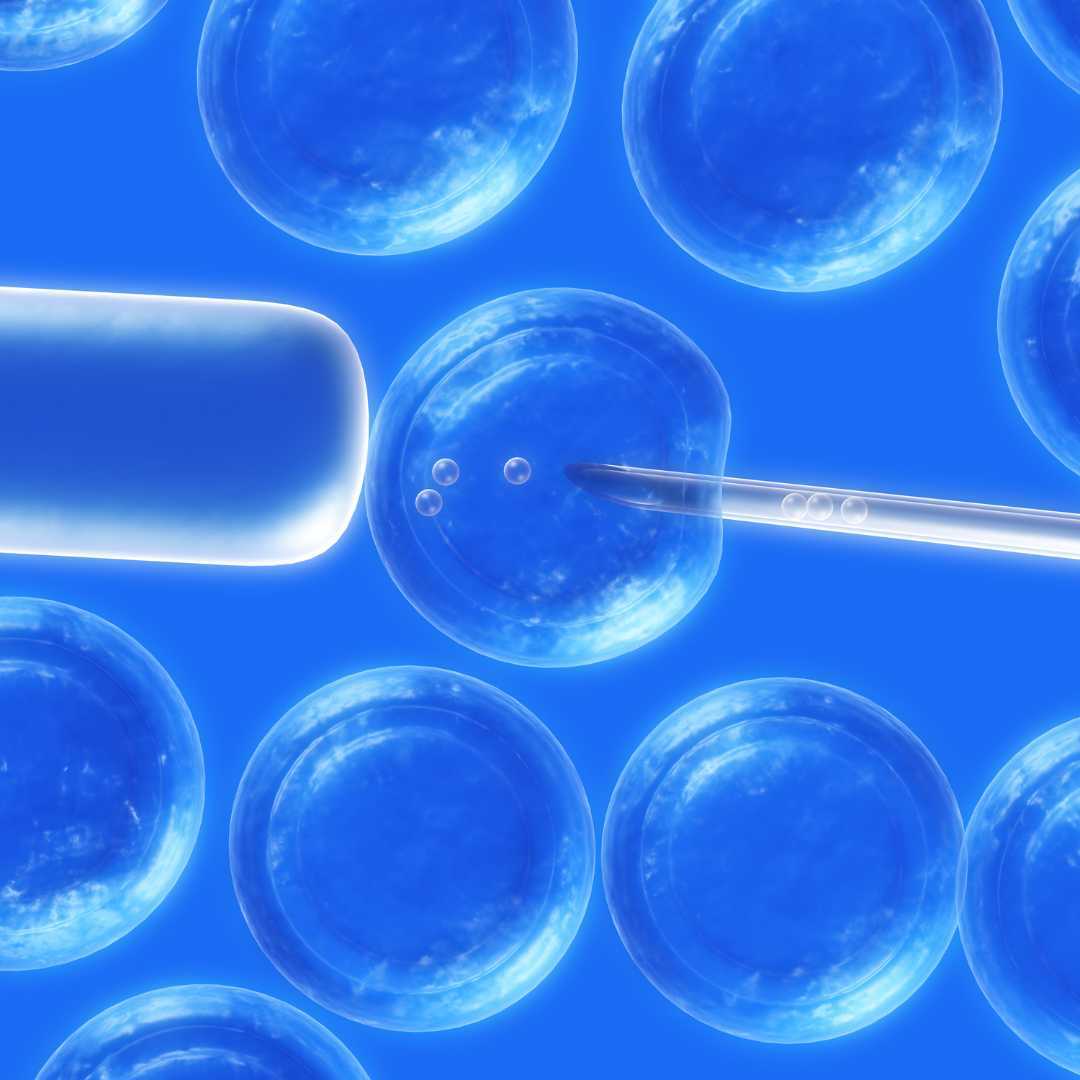
Gene therapy is like a biological "find and replace" tool. The most common approach involves taking a patient's own blood stem cells from their bone marrow. In a specialized lab, these cells are modified using a viral vector (a disarmed virus) that acts like a delivery truck, carrying a correct, functional copy of the hemoglobin gene into the cells' DNA. These newly "edited" and healthy stem cells are then infused back into the patient's body.
How does gene therapy work to cure thalassemia?
The process is intricate but can be broken down into a few key stages:
- Step 1: Cell Collection (Mobilization): First, the patient is given medication to encourage their blood stem cells to move from the bone marrow into the bloodstream. These cells are then collected from the blood in a process similar to donating plasma, called apheresis.
- Step 2: Gene Modification (Ex-vivo): This part happens outside the body (ex-vivo). The collected stem cells are sent to a high-tech lab. Here, scientists use a tool, typically a lentiviral vector, to deliver the correct gene into these cells.
- Step 3: Conditioning (Chemotherapy): Before receiving the modified cells, the patient undergoes a short course of chemotherapy. This is a crucial step that clears out space in the bone marrow, making room for the new, corrected stem cells to move in and set up shop.
- Step 4: Infusion: The modified stem cells, now containing the healthy gene, are given back to the patient through a simple IV infusion, much like a blood transfusion.
- Step 5: Engraftment: Over the next few weeks, these "super-cells" settle into the bone marrow (engraft) and begin to grow and multiply. They start producing new, healthy red blood cells that contain functional hemoglobin.
Over time, these healthy cells multiply and can produce enough hemoglobin for the patient to no longer need regular blood transfusions, effectively providing a gene therapy cure for thalassemia.
Is gene therapy a permanent cure for thalassemia?
This is what makes gene therapy so revolutionary. Unlike conventional treatments like blood transfusions, which only provide a temporary fix, gene therapy addresses the fundamental problem. Blood stem cells are incredibly long-lived and are the source of all new blood cells for your entire life.
By editing the DNA of these stem cells, the "fix" is passed down to all the cells they create. The goal is that after a single treatment, the body's own bone marrow will permanently produce enough healthy hemoglobin to end the need for transfusions and manage the disease's complications, such as iron overload. Clinical trials have shown that patients treated over a decade ago are still transfusion-independent.
What is the success rate of gene therapy for thalassemia?
These results are incredibly encouraging. For example, in the trials for Zynteglo (an approved gene therapy), a large majority of patients achieved "transfusion independence," meaning they no longer needed any red blood cell transfusions. Their bodies were producing enough of their own healthy hemoglobin to maintain safe levels.
The level of success can sometimes depend on the patient's specific genetic makeup (genotype) and age, but overall, the outcomes have been overwhelmingly positive. This high success rate is what led to the approval of these therapies by major health organizations like the FDA in the United States and the EMA in Europe.
Who is eligible for thalassemia gene therapy?
This treatment isn't for every person with thalassemia. The primary candidates are those with the most severe form, known as beta-thalassemia major or TDT, who rely on regular blood transfusions to survive.
Specific criteria often include:
- A confirmed diagnosis of transfusion-dependent beta-thalassemia.
- A "non-β0/β0" genotype (meaning they have at least one gene that produces some, albeit faulty, hemoglobin). However, therapies are also being approved for β0/β0 genotypes.
- No suitable or available "matched sibling" donor for a traditional bone marrow transplant.
- Patients must also be in general good health (aside from their thalassemia) to tolerate the conditioning chemotherapy.
As research expands, these eligibility criteria may broaden to include more patients, but for now, it's focused on those with the highest need.
What is the cost of gene therapy for thalassemia?
The staggering price tag is a major topic of discussion and a significant barrier to access. This cost covers the complex, multi-step process: cell collection, highly specialized lab work to modify the genes, the chemotherapy, the hospital stay, and long-term follow-up.
Proponents of the cost argue that it should be weighed against the lifelong cost of managing thalassemia with transfusions and chelation therapy, which can easily run into millions of dollars over a patient's lifetime, not to mention the impact on quality of life. However, this upfront cost presents a massive challenge for healthcare systems and insurance providers.
Cost Comparison: Gene Therapy vs. Lifelong Management
| Treatment Approach | Upfront Cost | Long-Term Cost (Estimated) | Key Considerations |
|---|---|---|---|
| Gene Therapy (e.g., Zynteglo) | ~$2.8 Million (One-time) | Minimal (Follow-up appointments) | Potential for a one-time cure. Eliminates need for transfusions. |
| Lifelong Transfusions & Chelation | Low (per treatment) | $5 Million - $10 Million+ (Lifetime) | Ongoing, lifelong treatment. Risk of iron overload. Significant time commitment. |
| Bone Marrow Transplant | $300,000 - $800,000 | Varies (Potential for long-term medication) | Requires a matched donor. Risk of Graft-vs-Host Disease (GvHD). |
Are there any risks or side effects of gene therapy for thalassemia?
It's important to understand that this is an intensive procedure. The chemotherapy (using a drug like busulfan) is necessary, but it's also what causes most of the short-term side effects. These can include:
- Infection Risk: The chemotherapy wipes out your immune system temporarily, leaving you highly vulnerable to infections until your new, modified cells grow back.
- Low Blood Counts: You will experience low platelets (risk of bleeding) and low red blood cells (anemia) and will require transfusions during this period.
- Infertility: The chemotherapy can damage sperm and eggs, leading to permanent infertility. Fertility preservation (sperm or egg freezing) is strongly recommended before starting the process.
- Theoretical Cancer Risk: There is a theoretical risk that the viral vector used to insert the gene could land in a "bad spot" in your DNA, potentially activating a cancer-causing gene. While this has been a concern, newer vectors are designed to be safer. Some cases of blood cancer have been reported in related trials (for sickle cell disease), so it remains a monitored risk.
How long is the recovery process after gene therapy?
The recovery timeline is dominated by the wait for engraftment. After the chemotherapy and the infusion of your modified stem cells, you are in a very vulnerable state. You will be in a protective isolation room in the hospital to prevent infection while you have no immune system.
During these weeks, doctors wait for the new cells to start producing white blood cells, red blood cells, and platelets. Once your blood counts reach a safe level, you can go home. However, your immune system will still be weak for many months, and you'll need to be careful to avoid illness. It can take 6 months to 2 years for your body to fully recover and for the full benefits of the treatment to be seen.
Is gene therapy for beta-thalassemia available now?
This is no longer just a futuristic concept; it's a clinical reality. The approval of Zynteglo marked a historic milestone for the thalassemia community. This means that if a patient meets the specific eligibility criteria, their doctor can prescribe this as a commercial treatment (pending insurance and hospital approval).
It is currently offered at a limited number of specialized "Qualified Treatment Centers" that have the expertise and facilities to handle the complex procedure. More gene therapies, including those using CRISPR gene therapy for thalassemia technology, are also in the final stages of clinical trials and may be approved soon.
What's the difference between gene therapy and a bone marrow transplant for thalassemia?
A bone marrow transplant (also called a hematopoietic stem cell transplant or HSCT) has been the only cure for thalassemia for a long time. It works by replacing the patient's faulty bone marrow with a healthy donor's, usually from a genetically matched sibling.
- Bone Marrow Transplant (Allogeneic):
- Pros: Proven, long-term cure.
- Cons: Requires a matched donor (hard to find), and carries a major risk of Graft-versus-Host Disease (GvHD), where the donor's immune cells attack the patient's body.
- Gene Therapy (Autologous):
- Pros: Uses the patient's own cells, so there is no need for a donor and no risk of GvHD.
- Cons: Requires the same intensive chemotherapy. It's a newer technology with less long-term (30+ year) data. Extremely high cost.
Gene therapy was developed specifically to overcome the two biggest hurdles of transplants: the need for a donor and the risk of GvHD.
How does CRISPR gene therapy for thalassemia work?
This is another, even more cutting-edge, form of gene therapy. We all have a gene for fetal hemoglobin (HbF), which we use in the womb, but it gets "switched off" shortly after birth when our bodies start making adult hemoglobin. In thalassemia, the adult hemoglobin gene is broken.
CRISPR (a gene-editing tool) is used to find the "off switch" (a gene called BCL11A) in the patient's blood stem cells and cut it. By disabling this switch, the cells "forget" to stop making fetal hemoglobin. They start producing large amounts of HbF again, which works perfectly well to carry oxygen and can free a patient from transfusion dependency. A treatment using this technology (Casgevy) has already been approved for sickle cell disease and is in trials for thalassemia.
What are the long-term effects of gene therapy for thalassemia?
The biggest long-term benefit is the elimination of chronic blood transfusions, which in turn stops the dangerous accumulation of iron in the body (iron overload). This can prevent organ damage to the heart, liver, and endocrine system, leading to a much healthier life and longer lifespan.
The main long-term risks being monitored are related to the chemotherapy (such as infertility) and the theoretical risk of cancer from the gene insertion. All patients who receive gene therapy are enrolled in long-term follow-up studies (often 15 years) to carefully monitor their health and ensure the treatment remains safe and effective for decades.
Can gene therapy help with alpha-thalassemia?
The genetics of alpha-thalassemia are more complicated. The disorder involves four gene alleles instead of two, and the most severe form (alpha-thalassemia major) is often fatal in the womb unless treated with in-utero transfusions.
Simply adding a new alpha-globin gene (like they do for beta-globin) is difficult because the amount of protein produced has to be very precisely controlled. Too much or too little can both cause problems. Scientists are actively working on it, but a commercially available gene therapy for alpha-thalassemia is still many years away.
What happens during the gene therapy procedure?
Here's a simplified timeline:
- Evaluation & Fertility Preservation (Month 1-2): You'll undergo extensive health screening. This is also when you would pursue sperm or egg freezing if you choose to.
- Mobilization & Collection (Month 3): You'll receive injections to push stem cells into your blood, then undergo apheresis to collect them. Your cells are then frozen and sent to the manufacturing lab.
- Manufacturing (2-3 Months): This is a waiting period. The lab uses the viral vector to insert the healthy gene into your stem cells and grows millions of copies.
- Hospital Admission & Conditioning (Month 6): You'll be admitted to the hospital. You will receive chemotherapy (e.g., busulfan) for several days to prepare your bone marrow.
- Infusion Day ("Day 0"): Your own modified cells are thawed and infused back into your vein. This part is simple and takes less than an hour.
- Hospital Recovery (4-6 Weeks): This is the long wait for engraftment, where you are monitored 24/7 for infection and low blood counts.
- Discharge & Home Recovery (Month 7+): You go home but remain in close contact with the hospital. Your immune system slowly rebuilds over the next 6-12 months.
Do I still need blood transfusions after gene therapy?
This is a common point of confusion. The chemotherapy wipes out your entire bone marrow, including its ability to make red blood cells. So, for the first one to two months after your infusion, you will be completely reliant on transfusions (both red cells and platelets) to stay alive while you wait for the new stem cells to "wake up" and take over.
As your new marrow starts to produce its own healthy red blood cells, your hemoglobin levels will slowly rise. Your doctor will monitor this, and if your levels become stable in a healthy range, they will stop scheduling your regular transfusions. For most patients in the trials, this milestone was reached within a few months of the procedure.
What are the approved gene therapies for thalassemia?
Zynteglo (beti-cel): This is the "gene addition" therapy that uses a lentiviral vector to insert a functional copy of the beta-globin gene. It's approved for adults and children with transfusion-dependent beta-thalassemia.
Casgevy (exa-cel): This is the "gene editing" therapy that uses CRISPR to turn on fetal hemoglobin production. It has been approved for sickle cell disease and is expected to receive full approval for transfusion-dependent beta-thalassemia as well, having shown excellent results in clinical trials.
What does the future hold for thalassemia gene therapy?
Scientists are working on major improvements. A key area of research is finding alternatives to the high-dose chemotherapy. They are testing "targeted conditioning" using antibodies that can clear the bone marrow without causing as much collateral damage to the rest of the body. This could potentially reduce or even eliminate risks like infertility.
Additionally, efforts are underway to streamline the manufacturing process to lower the astronomical cost of gene therapy for thalassemia. As the science of CRISPR and other editing tools becomes more precise, we can expect to see even better and safer thalassemia cures become available in the next decade.
Navigating advanced medical treatments like gene therapy can be overwhelming. You need a trusted partner to help you explore your options worldwide.
At PlacidWay, we are dedicated to connecting patients with world-class medical facilities and expert healthcare solutions. Whether you're seeking information on gene therapy, specialized treatments, or other advanced medical services, we are here to guide you.
Explore Your Healthcare Options with PlacidWay Today
.png)












Share this listing